The vesicula seminalis, also known as the seminal vesicle, is a glandular structure found in the male reproductive system. It plays a crucial role in the production of semen, which is the fluid that carries sperm during ejaculation.
What is vesicula seminalis?
It is a pair of convoluted tubular glands located behind the bladder and above the prostate gland in the male reproductive system. The seminal vesicles are responsible for secreting a significant portion of the fluid that makes up semen. This fluid, along with sperm from the testes and other secretions from the prostate gland and bulbourethral glands, forms semen, which is ejaculated during sexual intercourse. The seminal vesicle fluid contains various substances, including fructose, prostaglandins, enzymes, and other proteins, which nourish and support sperm, aiding in their survival and motility.
Functions
The seminal vesicles, or vesiculae seminales, play several important functions in the male reproductive system:
- Seminal Fluid Production: The primary function of the seminal vesicles is to produce and secrete seminal fluid, which is a major component of semen. Seminal fluid contributes a significant portion of the volume of ejaculate, typically around 60-70%. This fluid contains various substances that nourish, protect, and support sperm during their journey through the female reproductive tract.
- Fructose Secretion: Seminal vesicles secrete fructose, a type of sugar, into the seminal fluid. Fructose serves as an energy source for sperm cells, providing them with the fuel they need to sustain their motility and viability. This energy source helps sperm survive in the female reproductive tract and increases the likelihood of successful fertilization.
- Alkaline Secretion: The fluid produced by the seminal vesicles is alkaline in nature, meaning it has a higher pH. This alkalinity helps to neutralize the acidic environment of the male urethra and the female reproductive tract. By neutralizing acidity, seminal fluid ensures the survival and motility of sperm, as sperm are sensitive to acidic environments.
- Prostaglandin Production: Seminal vesicles also secrete prostaglandins, which are hormone-like substances that play various roles in the reproductive process. Prostaglandins help regulate smooth muscle contractions in the male and female reproductive tracts, aiding in sperm transport and facilitating fertilization.
Is seminal vesicle important organ and why?
Yes, the seminal vesicle is indeed an important organ in the male reproductive system for several reasons:
- Semen Production: The seminal vesicles produce and secrete a significant portion of the fluid that makes up semen. This fluid, along with sperm from the testes and other glandular secretions, forms semen. Semen provides a medium for sperm transport, protection, and nourishment, essential for successful fertilization.
- Nutrient Supply: Seminal vesicles secrete fructose, a type of sugar, into the seminal fluid. Fructose serves as an energy source for sperm cells, helping them maintain their viability and motility during their journey through the female reproductive tract. This nutrient supply is crucial for sperm survival and function.
- pH Regulation: The fluid produced by the seminal vesicles is alkaline, which helps to neutralize the acidic environment of the male urethra and the female reproductive tract. This alkalinity creates a more favorable environment for sperm survival and motility, enhancing the chances of successful fertilization.
- Prostaglandin Production: Seminal vesicles also secrete prostaglandins, which play various roles in the reproductive process. Prostaglandins help regulate smooth muscle contractions in the male and female reproductive tracts, aiding in sperm transport and facilitating fertilization.
- Fertility: Dysfunction or disorders of the seminal vesicles can lead to fertility issues in men. Problems such as inflammation, obstruction, or cancer of the seminal vesicles can affect semen quality and sperm function, potentially leading to infertility.
Location
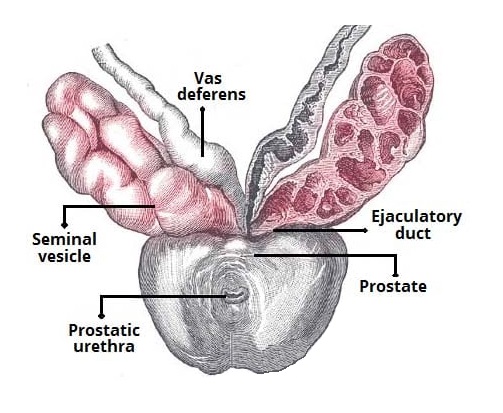
The seminal vesicles are located in the pelvis, specifically behind the bladder and above the prostate gland. They are paired structures, meaning there are two of them—one on each side of the midline. The seminal vesicles are positioned close to the base of the bladder and are connected to the vas deferens, which is the duct that carries sperm from the testes to the urethra.
Radiologic imaging
The best radiologic imaging modality for visualizing the seminal vesicles is typically magnetic resonance imaging (MRI) or transrectal ultrasound (TRUS).
- MRI: MRI provides detailed images of soft tissues, making it well-suited for visualizing the structures of the male pelvis, including the seminal vesicles. With MRI, it is possible to obtain high-resolution images that can show the size, shape, and any abnormalities of the seminal vesicles. Additionally, MRI can provide information about surrounding structures, helping to evaluate potential issues such as inflammation, obstruction, or tumors of the seminal vesicles.
- Transrectal Ultrasound (TRUS): TRUS is another imaging technique commonly used to assess the male reproductive system. During a TRUS procedure, a small ultrasound probe is inserted into the rectum to visualize the prostate gland and surrounding structures, including the seminal vesicles. TRUS can provide real-time images, allowing for dynamic evaluation of the seminal vesicles and nearby structures. It is often used in conjunction with other imaging modalities for a comprehensive assessment of the male reproductive system.
Examination of seminale vesicles
Examination of the seminal vesicles typically involves a combination of medical history, physical examination, and diagnostic tests. Here’s how a uroogist might approach the examination:
- Medical History: Urologists will start by taking a detailed medical history, including any symptoms you may be experiencing, such as pelvic pain, discomfort during ejaculation, blood in semen, or urinary symptoms.
- Physical Examination: During the physical examination, urologist may perform a digital rectal examination (DRE). Doctor may be able to assess the size, shape, consistency, and tenderness of the prostate gland and potentially detect any abnormalities suggestive of seminal vesicle involvement.
- Imaging Studies: Common imaging modalities used for this purpose include transrectal ultrasound (TRUS) and magnetic resonance imaging (MRI). These imaging studies can provide detailed images of the pelvic structures, including the seminal vesicles, and help detect any abnormalities such as inflammation, cysts, obstructions, or tumors.
- Laboratory Tests: In some cases, laboratory tests may be performed to assess semen quality or detect abnormalities. This may include semen analysis to evaluate sperm count, motility, and morphology, as well as tests to detect the presence of infection or blood in the semen.
- Additional Procedures: In certain situations, additional procedures may be recommended to further evaluate the seminal vesicles or surrounding structures. This may include cystoscopy or biopsy if cancer or other serious conditions are suspected.
Disorders
Disorders of the seminal vesicles can include various conditions that affect their structure or function. Some common disorders of the seminal vesicles include:
- Seminal Vesiculitis: This is inflammation of the seminal vesicles, often caused by bacterial infection. It can result in symptoms such as pelvic pain, discomfort during ejaculation, blood in semen (hematospermia), and sometimes fever. Seminal vesiculitis may be acute or chronic and can lead to complications such as abscess formation if left untreated.
- Seminal Vesicle Cysts: Cysts may form within the seminal vesicles, leading to pain or discomfort in the pelvic region. These cysts can be congenital (present from birth) or acquired and may require treatment if they cause symptoms or complications.
- Obstruction: Blockages in the ducts that drain the seminal vesicles can occur due to various reasons, such as inflammation, scarring, or anatomical abnormalities. Seminal vesicle obstruction can result in impaired semen quality, infertility, or discomfort.
- Seminal Vesicle Stones: Calcifications or stones may develop within the seminal vesicles, causing pain and potentially obstructing the flow of semen. These stones can sometimes be detected on imaging studies and may require treatment if they cause symptoms.
- Congenital Abnormalities: Rarely, congenital abnormalities of the seminal vesicles may be present, such as absence of one or both seminal vesicles (agenesis), duplication, or malformation. These abnormalities may be associated with other congenital anomalies of the genitourinary system.
- Tumors: Although rare, tumors can develop within the seminal vesicles. These tumors can be benign (such as cystadenomas) or malignant (such as adenocarcinomas). Symptoms may include blood in semen, painful ejaculation, pelvic pain, or urinary symptoms.
Cancers commonly invade to seminal vesicle
Cancers that commonly invade or spread to the seminal vesicles include:
- Prostate Cancer: Prostate cancer is the most common cancer that can involve the seminal vesicles. Prostate cancer cells can extend beyond the prostate gland and invade surrounding structures, including the seminal vesicles. Seminal vesicle invasion by prostate cancer is typically seen in advanced or aggressive cases and may indicate a higher stage of the disease.
- Bladder Cancer: In some cases, bladder cancer can extend into nearby structures, such as the seminal vesicles, especially if the cancer is locally advanced. Direct invasion of the seminal vesicles by bladder cancer is less common than prostate cancer involvement but can occur in certain cases.
- Rectal Cancer: Rectal cancer is another malignancy that can potentially invade the seminal vesicles, particularly if the cancer is located in the lower part of the rectum and extends into the surrounding pelvic structures. Invasion of the seminal vesicles by rectal cancer may indicate locally advanced disease.
- Metastatic Cancer: Cancers from distant sites in the body (metastatic cancers) can sometimes spread to the seminal vesicles as part of advanced metastatic disease. Common primary cancers that may metastasize to the seminal vesicles include cancers of the prostate, bladder, rectum, and other pelvic organs.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul -TURKIYE



Leave a Reply