Testicular Cancer Surgery
Testicular cancer is a malignant tumor arising from the testicle. It is usually seen unilaterally and on the right, rarely seen in both testicles. It is mostly seen at young ages. In this article, I will give general information about testicular cancer surgery, taking into account my own experiences.
What is testicular cancer?
Testicular cancer is cancer that originates in the testicles in men. Cancers that metastasize to the testis, that is, develop from other organs and then spread to the testis, are extremely rare. Generally, when we say testicular cancer, primary testis, that is, cancers that develop directly from the testicular tissue, is understood.
What are the types of testicular cancer?
Cancers that develop from the own tissue of the testis are divided into different subgroups histologically (pathology). Testicular cancer is divided into two main groups;
- Seminoma
- Classical seminoma
- Spermatocytic seminoma
- Anaplastic seminoma
- Non-seminoma testicular cancers
- Embryonal carcinoma
- Choriocarcinoma
- Teratoma
- Yolk sac tumor
Apart from these, tumors may develop from the supporting tissues in the testis. These tumors are extremely rare. Cancers that develop from the supporting tissues of the testis are of two main types;
- Leydig cell cancers
- Sertoli cell cancers
What are the symptoms of testicular cancer?
Patients with testicular cancer have complaints according to the stage of the disease. While there are not many symptoms other than swelling in the testis in the early stages, the symptoms differ according to the location in the advanced stages.
- Testicular swelling (growth, mass): The most important symptom of testicular cancer is painless, hard growth (swelling) in the testis. Sometimes pain can occur in cases of bleeding into the cancer, torsion (turning of the testis around itself) or trauma. Sometimes, blood may come from the semen as a result of ejaculation during intercourse. Since these patients do not have pain, they usually apply to the doctor late. This causes the progression of the disease. In this regard, if there is painless enlargement and stiffness in the testis, it is absolutely necessary to consult a urologist. Sometimes the enlargement and stiffness in the testis is noticed by the spouse or partner of the patient. Testicular cancer often occurs between the ages of 15-40. The incidence of testicular cancer in advanced ages is very low.
- Bone pain: If the cancer is very advanced and has spread to the bones, there may be bone pain.
- Bloody sputum, cough: One of the places where testicular cancer spreads frequently is the lungs. In patients with lung spread (metastasis), blood in the sputum and cough may be seen.
- Abdominal pain, nausea and vomiting: If testicular cancer progresses and spreads to the lymph nodes in the posterior abdominal wall (retroperitoneal region), abdominal pain, nausea and vomiting may occur as it will compress the intestines.
- Swelling in the legs: As a result of testicular cancer pressing on the lymph nodes, blood circulation from the legs is prevented and swelling occurs.
What are the causes of testicular cancer?
Sometimes no cause can be found in test cancer, which is mostly seen at a young age. In most patients, some generally known factors are important in the development of cancer. The most common causes of testicular cancer are:
- Undescended testis (cryptorchidism): Sometimes congenital testicles are not in their normal place. It stays in the groin or in the abdomen. These conditions pose a risk for testicular cancer.
- It can be familial: Like many other cancers, testicular cancer also has a familial aspect.
- Atrophic (small) testis: Cancer may develop after a long time in testicular atrophy due to infection or trauma.
How is testicular cancer diagnosed?
The diagnosis of testicular cancer is easy. In order to diagnose our patients who come to us with a mass (swelling) in the testis, we perform the following procedures;
- Questioning the patient: Patients are generally subjected to medical questioning. Conditions that may cause testicular cancer are investigated.
- Examination of the patient: Testicular examination is done while standing. Both testicles are evaluated. Testicular consistency, pain, swelling are checked. If there is a painless and hard mass (swelling), cancer should be suspected.
- Blood tests in testicular cancer: There are 3 important cancer markers called “markers” that help in the diagnosis of testicular cancers. These should definitely be done in the blood of those who are suspected of cancer. 3 important markers of testicular cancer: Beta HCG, Alpha fetoprotein, Lactic dehydrogenase. These tests do not increase in all types of cancer, they may increase depending on the type and prevalence of cancers. In some types of cancer, it can be found completely normal.
- Radiological diagnostic methods: We make significant use of radiological tests for the purpose of diagnosing and staging cancer. We can list these tests as follows;
USG: Diagnosis is easily made with USG (testicular ultrasonography).
MRI-CT: It is mostly used in metastasis research in testicular cancers in advanced stages. Since testicular cancers frequently spread to the lymph nodes and lungs in the abdomen and posterior part of the abdomen, these areas should be investigated primarily.
PET-CT: It is used in the investigation of metastasis.
How to prepare before testicular cancer surgery?
Patients diagnosed with testicular cancer should not wait too long for surgery. If the examination, blood tests (tumor markers) and radiological tests show that there is cancer, surgery is performed as soon as possible without waiting too long. Patients do not eat or drink anything by mouth 4-5 hours before the operation, routine blood tests are taken for anesthesia. Generally, since these patients are young, there is no obstacle to surgery.
How long is the operation time, type of anesthesia and hospital stay?
Testicular cancer surgery (high inguinal radical orchiectomy) takes about 45 minutes. The surgery is performed under general anesthesia or spinal anesthesia. Patients are discharged the same day or stay in the hospital overnight.
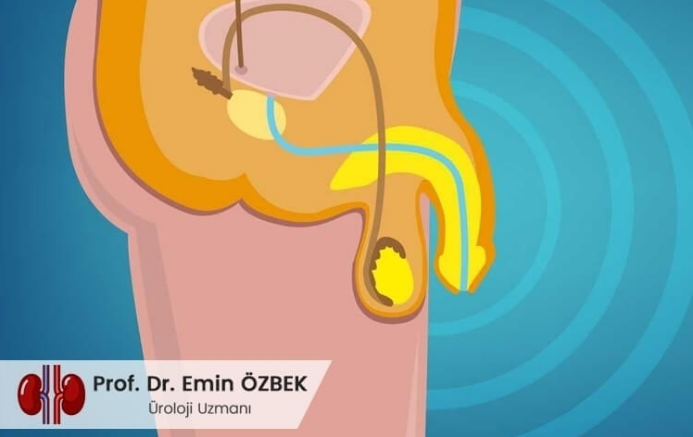
How is testicular cancer surgery performed?
Surgery to remove the cancerous testis due to testicular cancer is called “high inguinal radical orchiectomy” surgery. For this surgery, patients are placed on their backs after being put to sleep. It is opened with an incision of 3-4 cm from the inguinal region, and the spermatic cord (the structure where the testicular vessels and semen canals are located) is found and tied and cut. The cancerous testicle is released from the scrotum and taken out. Follow the bleeding control, incision is closed in accordance with the procedure.
In testicular cancer surgery, the incision must be made from the groin, not from the scrotum. This is because the lymphatic system of the testicles is impaired and the cancer may spread to the lower lymph nodes. Since we cover the surgical site with aesthetic sutures, there is usually no scar.
Additional treatments may be required depending on the pathology and intra-abdominal lymph involvement and metastasis after surgery. (such as radiation therapy, radiotherapy, retroperitoneal lymph node dissection).
What is “retroperitoneal lymph node dissection” surgery in testicular cancer?
Retroperitoneal lymph node dissection (RPLND) is the operation of surgical removal of lymph nodes in this region in case of testicular cancers in the lymph nodes called retroperitoneal lymph nodes in the abdomen. The lymph nodes of the testis are located around the kidney and around the great vessels (aorta, vena cava) in the back of the abdomen.
Sometimes the disease can also envelop the main arteries and veins in this region. In this case, a serious operation involving cardiovascular surgery is required.
What should be considered after the operation?
After the surgery, patients do not eat or drink orally for 4-5 hours. They are fed intravenously. During this period, the patient is given intravenous serum and painkillers are administered. 4-5 hours after the effect of anesthesia wears off, patients start to take water and soft foods by mouth, stand up and walk. We usually discharge our patients the same day or keep them in the hospital for 1 night. After 4-5 days of rest after the operation, the patients start their normal work. It is better not to work hard for more than 1 month and not to do heavy sports.
After the pathology result is obtained, additional treatments (radiation therapy, chemotherapy) may be required depending on the stage of the disease and the type of cancer. The doctor calls his patients for control at regular intervals in certain periods.
When should patients call their doctor after surgery?
Testicular cancer surgeries are usually uneventful, and post-operative emergency problems that require hospitalization are rarely seen. If there is excessive swelling, bruising, pain at the surgery site, and high fever, patients should definitely call their doctor.
Is testicular prosthesis inserted after testicular cancer surgery?
In patients whose testis is removed due to testicular cancer, the bag (scrotum) on that side will be empty, and there may be psychological problems in the patients. To prevent this, prostheses made of special silicone in the shape and size of testicles are placed on the scrotum, giving an appearance as if there is a normal testicle and psychologically relieves the patient. The testicular prosthesis has no secretory function.
It does not produce sperm, does not secrete testosterone. It is for aesthetic purposes only. Since testicular cancer patients are young patients, replacing the removed testicle with a prosthesis will give the patients a serious morale boost. If there is cancer in two testicles and both have been removed, it would be more appropriate to put a bilateral testicular prosthesis.
Testicular prosthesis can be done in the same session as the cancer surgery, or it can be done later. It is better for the patient to do it in the same session. After the cancerous testicle is removed while receiving anesthesia, a testicular prosthesis is placed in its place.
Can testicular cancer patients have infertility and erectile dysfunction?
Before surgery, chemotherapy and radiation therapy, patients with testicular cancer should be asked whether they have children and whether they would like to have children.
Since surgical removal of the testis, chemotherapy and radiation therapy will adversely affect the sperm, these sperm can be used in in vitro fertilization treatment if patients want to have children in the later periods by giving sperm to sperm banks before these procedures.
If the male hormone is normal, it is usually normal in unilateral cancers, there are no impotence problems. If there is cancer in both testicles and both are removed, then testosterone deficiency and eventually sexual problems will occur. Such patients should be treated with testosterone therapy. This treatment is a lifelong treatment.
In summary; Testicular cancer is a malignant manifestation of the testis in young men. The most important symptom is painless testicular enlargement. If the diagnosis of cancer is confirmed, the cancerous testis must be surgically removed. If there is a spread to the lymph nodes, RPLN surgery may be required. Depending on the stage of the disease, drug or radiation therapy is performed. After the testicle is removed, a testicular prosthesis can be inserted for aesthetic purposes in the same session or in place of the testicle taken later. Patients should be informed about infertility.
Prof. Dr. Emin ÖZBEK
Urology Specialist
Istanbul- TURKEY

