Testicular microlithiasis (TM) is a condition characterized by the presence of tiny calcium deposits within the testes. It is typically asymptomatic and discovered incidentally during ultrasound (USG) examinations conducted for other reasons, such as investigating testicular pain, swelling, or infertility. While testicular microlithiasis itself is benign and does not require treatment, its presence may be associated with an increased risk of testicular cancer and other testicular conditions, warranting regular monitoring and proactive healthcare practices.
What is “testicular microlithiasis”?
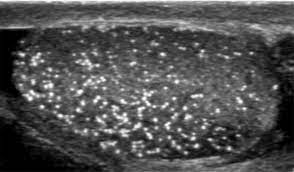
Testicular microlithiasis is a medical condition characterized by the presence of tiny calcifications, or small clusters of calcium deposits, within the testes. These calcifications are usually detected through an USG examination and appear as small, bright spots on the imaging results.
It is most often discovered incidentally during ultrasounds conducted for other reasons, as it typically does not cause symptoms. It is a relatively rare condition and can occur in males of any age, though it is more commonly found in younger men.
Causes
The exact cause of TM is not fully understood, but several factors and conditions have been associated with its presence. Here are some possible causes and associated conditions:
Genetic Factors: There may be a genetic predisposition to developing testicular microlithiasis, although specific genetic markers have not been definitively identified.
Testicular Trauma or Inflammation: Past trauma or inflammation of the testes, such as from infections or injuries, may contribute to the formation of microliths.
Testicular Dysgenesis: Conditions that affect the normal development of the testes, such as cryptorchidism (undescended testes) or Klinefelter syndrome, have been linked to testicular microlithiasis.
Hormonal Imbalances: Hormonal imbalances during fetal development or later in life may play a role in the development of microlithiasis.
Environmental Factors: Exposure to certain environmental toxins or factors during critical periods of testicular development might contribute to the condition.
Association with Other Testicular Conditions: TM has been found in association with various testicular conditions, including:
- Testicular Cancer
- ,Infertility
- Varicoceles
- Infectious Diseases
Clinical significance
The clinical significance of TM lies in its potential associations with other medical conditions and implications for patient management. Here are the key points regarding its clinical significance:
- Association with Testicular Cancer: There is ongoing debate about the potential association between TM and an increased risk of testicular cancer. Some studies suggest that men with TM, especially those with additional risk factors such as a family history of testicular cancer or previous testicular cancer, may have a higher risk.
- Infertility: TM has been found in higher prevalence among men undergoing evaluation for infertility. It is thought that the presence of microliths may be indicative of underlying testicular dysfunction.
- Testicular Dysgenesis Syndrome (TDS): TM can be part of a spectrum of conditions associated with TDS, which includes cryptorchidism (undescended testes), hypospadias, poor semen quality, and testicular cancer.
- Testicular Inflammation and Infections: TM may be associated with a history of testicular inflammation or infections, such as mumps orchitis.
- Varicoceles: There is some evidence to suggest a correlation between TM and the presence of varicoceles.
Management and follow-up
Due to the potential associations with other conditions, particularly testicular cancer, men diagnosed with TM are often advised to:
- Perform Regular Self-Examinations: Regularly check the testicles for any new lumps, changes in size, or other abnormalities.
- Follow-Up USG: Undergo periodic ultrasound examinations to monitor for any changes in the testicles.
- Consult Urologist: Seek medical advice if any symptoms or abnormalities are noticed.
Symptoms
TM itself does not typically cause symptoms. It is usually discovered incidentally during ultrasound examinations conducted for other reasons, such as investigating infertility, testicular pain, or swelling. Here are the primary points to understand about the symptoms (or lack thereof) of TM:
No Direct Symptoms: TM is generally asymptomatic, meaning it does not cause any noticeable symptoms or discomfort directly attributable to the calcifications themselves.
Associated Conditions: While TM does not cause symptoms directly, it can be associated with conditions that might produce symptoms:
- Testicular Cancer
- Infertility
- Varicoceles
- Testicular Inflammation or Infection
Psychological impact: Awareness of having TM, especially given its potential associations, can cause anxiety and stress. Providing appropriate counseling and education to patients is important to alleviate concerns and promote proactive health management.
Diagnosis
The diagnosis of TM primarily involves imaging techniques, particularly ultrasound, as the condition is typically asymptomatic and discovered incidentally. Here’s an overview of how TM is diagnosed:
Medical History and Physical Examination:
- Medical History: A urologist will take a detailed medical history, including any past testicular issues, family history of testicular cancer, infertility, and other relevant health concerns.
- Physical Examination: A thorough physical examination of the testicles and scrotum will be conducted to check for any lumps, swelling, or other abnormalities.
Scrotal Ultrasound:
- Primary Diagnostic Tool: Scrotal ultrasound is the primary diagnostic tool for detecting TM. It uses high-frequency sound waves to create detailed images of the testicles.
- Appearance on Ultrasound: TM appears as multiple tiny, bright (hyperechoic) foci within the testicles. These microliths are typically less than 3 mm in size and do not cast acoustic shadows.
- Criteria: The diagnosis is generally confirmed when multiple microliths are detected in one or both testicles. There is no universally agreed-upon threshold for the number of microliths, but some criteria suggest the presence of five or more microliths in at least one testicle.
Additional Diagnostic Tests (if indicated):
- Tumor Markers: In cases where there is concern about testicular cancer, blood tests for tumor markers such as alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH) may be performed.
- Further Imaging: If a suspicious mass is detected on ultrasound, additional imaging studies like MRI or CT scans may be recommended to further evaluate the testicles and surrounding structures.
Prognosis
The prognosis of TM is generally favorable, especially since the condition itself is benign and typically asymptomatic. However, the presence of TM has potential implications that warrant careful monitoring and management. Here’s an overview of the prognosis:
Benign Nature of TM
- Asymptomatic and Non-progressive: TM is usually asymptomatic and does not progress to cause symptoms or direct harm. The calcifications themselves remain stable and do not require treatment.
Potential Association with Testicular Cancer
- Increased Risk: Some studies suggest an increased risk of testicular cancer in individuals with TM, particularly in those with additional risk factors such as a history of cryptorchidism (undescended testes), family history of testicular cancer, or personal history of testicular cancer.
- Monitoring and Early Detection: With regular monitoring, including testicular self-examinations and periodic ultrasounds, any development of testicular cancer can potentially be detected early when it is most treatable.
Infertility
- Association with Infertility: There is an observed association between TM and male infertility. Men with TM may have underlying testicular dysfunction that could affect fertility.
- Evaluation and Treatment: Men experiencing infertility should undergo a comprehensive evaluation to determine the underlying cause and appropriate treatment options. TM itself does not cause infertility, but its presence can indicate other testicular issues.
Treatment
TM is generally a benign condition that does not require treatment in itself. The management approach focuses primarily on monitoring and addressing any associated risks or underlying conditions. Here’s an overview of the recommended management and follow-up strategies:
Observation and Monitoring
- Regular Ultrasound Examinations: Periodic scrotal ultrasounds may be recommended to monitor for any changes or developments in the testicles, especially if there are additional risk factors for testicular cancer.
- Testicular Self-Examination: Patients are advised to perform regular testicular self-examinations to detect any new lumps, swelling, or changes early. This practice is crucial for early detection of testicular cancer.
Risk Assessment and Surveillance
- Risk Stratification: Based on individual risk factors such as a history of cryptorchidism, family history of testicular cancer, or previous testicular cancer, a tailored surveillance plan may be developed.
- Follow-Up Schedule: The frequency of follow-up ultrasounds and clinical evaluations will depend on the individual’s risk profile. Those with higher risk may require more frequent monitoring.
Addressing Associated Conditions
- Infertility Evaluation: Men with TM who are experiencing infertility should undergo a thorough evaluation to identify any underlying causes. This may include semen analysis, hormonal tests, and other relevant investigations.
- Treatment of Underlying Conditions: If TM is associated with other testicular abnormalities or conditions (e.g., varicoceles, testicular inflammation), appropriate treatment for those conditions should be provided.
Education and Counseling
- Patient Education: Informing patients about the nature of TM, its benign nature, and the importance of regular monitoring helps reduce anxiety and ensures proactive health management.
- Counseling: Psychological support and counseling may be beneficial for patients who are anxious about the potential implications of TM, particularly the possible increased risk of testicular cancer.
Management of Testicular Cancer Risk
- Proactive Monitoring: For those at higher risk of testicular cancer, more intensive surveillance may be recommended, including regular clinical evaluations by a urologist.
- Early Detection: Emphasis on early detection through self-examination and regular medical check-ups is crucial for managing the potential risk of testicular cancer.
Summary
TM is a benign condition characterized by the presence of small calcium deposits within the testicles. It is typically asymptomatic and often discovered incidentally during ultrasound examinations. While TM itself does not require treatment, it may be associated with an increased risk of testicular cancer, infertility, and other testicular conditions. Management involves regular monitoring through ultrasound and testicular self-examination to detect any changes early.
Prof Dr. Emin ÖZBEK
Urologist
Istanbul – TURKIYE



Leave a Reply