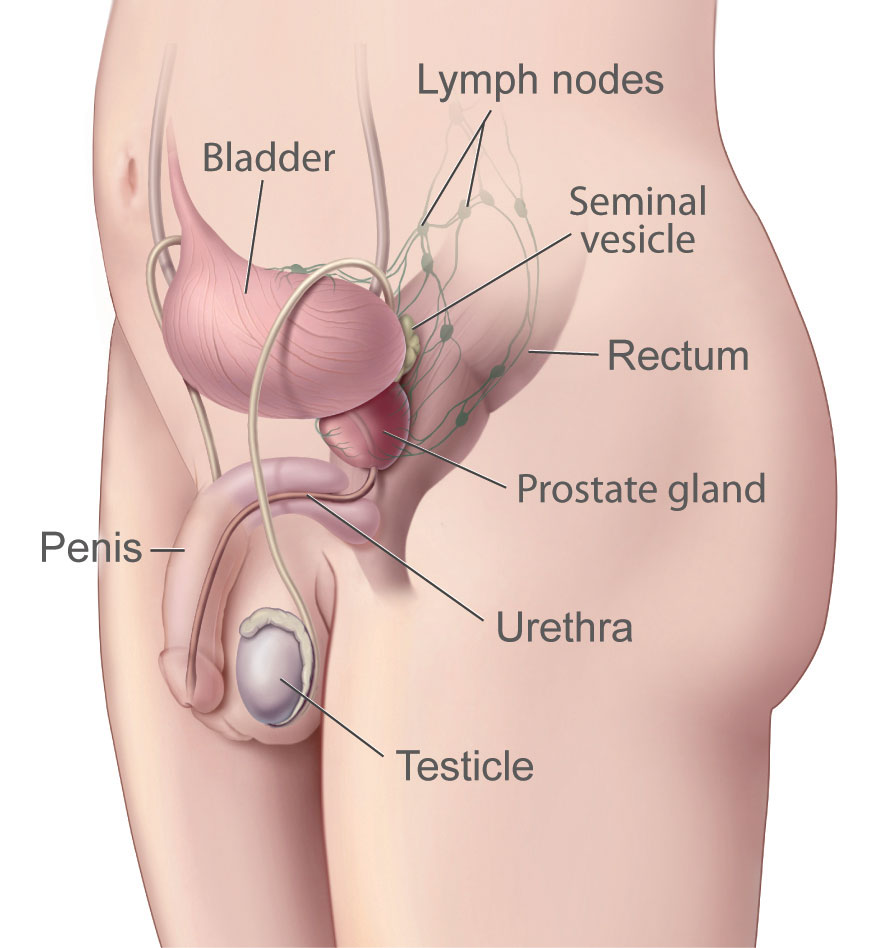
The prostate is a small, walnut-shaped gland located below the bladder and in front of the rectum in men. It surrounds the urethra, the tube through which urine and semen exit the body. The prostate plays a crucial role in the male reproductive system.
The prostate is composed of several zones, including the peripheral, central, and transition zones. The gland is enclosed in a capsule and has a rich supply of blood vessels and nerves. Main function of the prostate is to produce and secrete a fluid that forms part of semen. Common prostatic diseases are benign prostatic hyperplasia (bph): prostatitis and prostate cancer.
I will provide general information about the prostate in this article.
What is prostate?
The prostate is a small gland in the male reproductive system. It is approximately the size of a walnut and is located below the bladder and in front of the rectum. The prostate surrounds the urethra, the tube that carries urine from the bladder and semen from the reproductive system out of the body through the penis.
The primary role of the prostate is to produce a fluid that, together with sperm cells from the testes and fluids from other glands, makes up semen. This prostatic fluid is slightly alkaline and helps to nourish and protect sperm, aiding their mobility and survival as they travel through the female reproductive tract.
In addition to its reproductive function, the prostate also plays a role in urinary control. It contains muscular tissue that helps in the regulation of urine flow by contracting and relaxing around the urethra. This dual role makes the prostate an essential gland for both reproductive and urinary health in men.
Anatomy of the prostate
The prostate is a complex gland with a distinct anatomical structure, playing a vital role in the male reproductive system. Here’s a detailed overview of its anatomy:
Structure
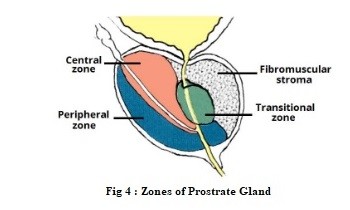
Zones of the Prostate
- Peripheral Zone (PZ): This is the largest zone, comprising about 70% of the prostate. It is located at the back of the gland, near the rectum, and is where most prostate cancers originate.
- Central Zone (CZ): This zone surrounds the ejaculatory ducts and makes up about 25% of the prostate. It is relatively resistant to disease compared to the peripheral zone.
- Transition Zone (TZ): This zone surrounds the urethra and is the site where benign prostatic hyperplasia (BPH) commonly occurs. It constitutes about 5% of the prostate in young men but can grow significantly with age.
Fibromuscular Stroma
- This is a non-glandular area located at the front of the prostate, composed of fibrous and muscular tissue. It helps support the gland and plays a role in its contraction during ejaculation.
Glandular Structure
- The prostate consists of numerous small glands that secrete prostatic fluid. These glands open into ducts that converge into larger ducts, eventually emptying into the urethra.
- The glandular tissue is embedded in a matrix of connective tissue and smooth muscle, which helps expel the prostatic fluid during ejaculation.
Capsule
- The prostate is surrounded by a thin, fibrous capsule that provides a protective layer. This capsule also contains blood vessels and nerves, contributing to the gland’s rich blood supply and innervation.
Blood Supply and Innervation
- Blood Supply: The prostate receives blood primarily from the inferior vesical artery, a branch of the internal iliac artery. The blood supply is essential for the gland’s function and health.
- Innervation: The prostate is innervated by the autonomic nervous system, with sympathetic and parasympathetic fibers contributing to its function. These nerves are crucial for regulating prostatic secretion and contraction during ejaculation.
Location and relationship to other structures
The prostate is located in the male pelvis. Here are some key details about its location:
- Below the Bladder: The prostate is situated directly beneath the urinary bladder. It encircles the urethra, which is the tube that carries urine from the bladder out of the body.
- In Front of the Rectum: The prostate lies in front of the rectum, making it accessible for examination through a digital rectal exam (DRE).
- Above the Urogenital Diaphragm: It rests above the urogenital diaphragm, a layer of muscle and connective tissue that supports the pelvic organs.
- Surrounding the Urethra: The prostate surrounds the prostatic urethra, the section of the urethra that runs through the prostate gland. This positioning allows the prostate to release its fluid into the urethra, where it mixes with sperm and other seminal fluids during ejaculation.
Functions of the prostate?
The prostate gland plays several important roles in the male reproductive system and overall health. Here are the primary functions of the prostate:
Production of Prostatic Fluid
- Component of Semen: The prostate produces a fluid that constitutes about 20-30% of the total volume of semen. This fluid is slightly alkaline, which helps to neutralize the acidity of the vaginal tract and prolongs the lifespan of sperm.
- Nourishment and Protection of Sperm: Prostatic fluid contains enzymes, proteins, and minerals that support and protect sperm cells, enhancing their motility and viability.
Support in Ejaculation
- Muscular Contraction: The smooth muscle tissue within the prostate contracts during ejaculation, helping to expel semen through the urethra. This process ensures the proper mixing of prostatic fluid with sperm and other seminal fluids.
Urinary Control
- Urethral Support: The prostate surrounds the urethra, providing structural support and playing a role in controlling the flow of urine. The muscle fibers in the prostate help maintain urinary continence by preventing the backward flow of urine.
Hormonal Conversion
- Conversion of Testosterone: The prostate contains the enzyme 5-alpha-reductase, which converts testosterone into dihydrotestosterone (DHT). DHT is a more potent form of testosterone that plays a role in the development and maintenance of male characteristics and prostate growth.
Antimicrobial Action
- Defense Mechanism: Prostatic fluid contains antimicrobial compounds that help reduce the risk of infections in the urinary tract and reproductive system.
Common diseases of the prostate
The prostate can be affected by several common diseases, particularly as men age. Here are the most prevalent prostate conditions:
Benign Prostatic Hyperplasia (BPH): BPH is a non-cancerous enlargement of the prostate gland. It is common in older men and can cause various urinary symptoms due to the compression of the urethra.
Prostatitis: Prostatitis is inflammation of the prostate gland, which can be acute or chronic. It can be caused by bacterial infections or occur without an identifiable infectious agent. There are different types of prostatitis: Acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (cp/cpps), asymptomatic ınflammatory prostatitis:
Prostate Cancer: Prostate cancer is one of the most common cancers in men. It often grows slowly and may not cause symptoms in its early stages. Early detection through screening is critical for effective treatment.
Diagnostic tests for prostatic diseases
Diagnosing prostatic diseases involves a combination of clinical evaluations, laboratory tests, and imaging studies. Here are the common tests used to diagnose prostate conditions:
Prostate-Specific Antigen (PSA) Test: A blood test that measures the level of PSA, a protein produced by the prostate gland.
Digital Rectal Exam (DRE): A physical examination where a healthcare provider inserts a gloved, lubricated finger into the rectum to feel the size, shape, and texture of the prostate.
Urinalysis and Urine Culture: Laboratory tests that analyze urine samples to check for signs of infection, blood, or other abnormalities.
Prostate Biopsy: A procedure where small samples of prostate tissue are removed using a needle for microscopic examination.
Transrectal Ultrasound (TRUS): An imaging test that uses sound waves to create images of the prostate. Helps evaluate prostate size, guide biopsies, and assess any abnormalities detected during a DRE or elevated PSA levels.
Magnetic Resonance Imaging (MRI): A non-invasive imaging technique that provides detailed images of the prostate and surrounding tissues. Used to evaluate prostate cancer, particularly in planning biopsies and staging cancer. MRI can help determine the extent of cancer spread and guide treatment decisions.
Urodynamic Tests: A series of tests that measure how well the bladder and urethra store and release urine. Helpful in assessing urinary symptoms associated with BPH or other urinary disorders.
Cystoscopy: A procedure where a thin, flexible tube with a camera is inserted into the urethra to view the bladder and prostate. Used to evaluate urinary symptoms and visualize any obstruction or abnormality in the lower urinary tract.
These tests are often used in combination to accurately diagnose prostatic diseases and determine the most appropriate treatment plan. Regular check-ups and screenings are important for early detection and management of prostate conditions.
Radiological Imaging
Main radiologic tests to diagnose prostatic diseases are:
- Transrectal Ultrasound (TRUS)
- Magnetic Resonance Imaging (MRI)
- Computed Tomography (CT) Scan
Radionuclide Imaging
Main radiologic tests to diagnose prostatic diseases are:
- Prostate-Specific Membrane Antigen (PSMA) PET Scan
- Bone Scan
Summary
The prostate is a small, walnut-shaped gland in the male reproductive system, located below the bladder and in front of the rectum. It surrounds the urethra, the tube that carries urine and semen out of the body. The prostate is divided into several zones. The prostate gland has several important functions, including: Production of seminal fluid, protection of sperm, regulation of urine flow, hormone metabolism. Common prostate diseases: Benign prostatic hyperplasia (bph), prostatitis and prostate cancer.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE



Leave a Reply