Chemotherapy-induced male infertility is a significant concern for men undergoing cancer treatment. Chemotherapy, while effective in targeting cancer cells, can adversely affect sperm production and quality, leading to potential infertility. Understanding the impact of chemotherapy on male reproductive health, as well as exploring options for preserving fertility, is crucial for providing comprehensive care and support to patients.
This introduction explores the mechanisms by which chemotherapy affects male fertility, the implications for patients, and strategies for managing and mitigating these effects.
Incidence of chemotherapy induced male intfertility
The risk of chemotherapy-induced male infertility varies widely based on several factors, with incidence rates ranging from 10% to 90% depending on the treatment specifics. For individuals undergoing chemotherapy, discussing fertility preservation options with urologists is crucial prior to the start of treatment.
Mechanisms of chemotherapy induced male infertility
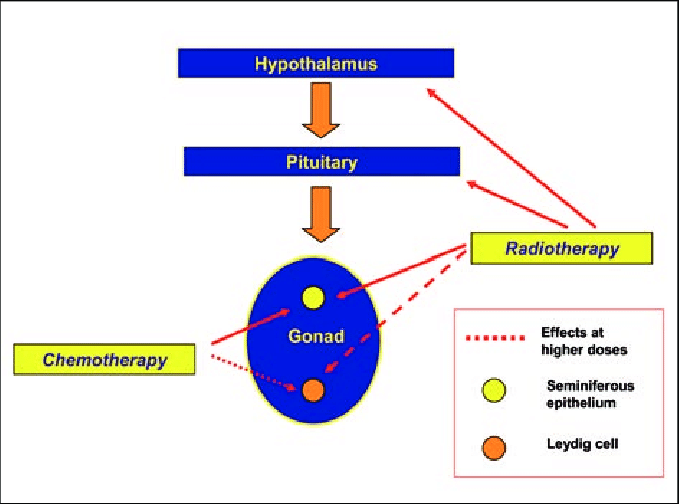
Chemotherapy-induced male infertility and sperm dysfunction primarily result from the detrimental effects of chemotherapy drugs on the male reproductive system. The main mechanisms involved include:
- Damage to Spermatogenic Cells: Chemotherapy drugs target rapidly dividing cells, which includes spermatogenic cells in the testes responsible for sperm production. This damage can lead to reduced sperm count and quality.
- Hormonal Disruption: Chemotherapy can alter the balance of hormones necessary for spermatogenesis, including testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). Hormonal imbalances can impair sperm production and function.
- Testicular Toxicity: Some chemotherapy agents have direct toxic effects on the testicular tissues, leading to decreased sperm production and altered sperm morphology.
- Oxidative Stress: Chemotherapy can increase oxidative stress within the reproductive system, leading to damage to sperm DNA and affecting sperm motility and viability.
- Apoptosis: The drugs may induce apoptosis (programmed cell death) in spermatogenic cells, further reducing sperm production and contributing to infertility.
- Impact on Testicular Vasculature: Chemotherapy may affect blood flow to the testes, impairing their ability to maintain a healthy environment for sperm production.
Chemotherapeutic agents cauce male infertility
Several chemotherapeutic agents are known to cause male infertility due to their effects on spermatogenesis and testicular function. Key agents include:
- Alkylating Agents: These are among the most commonly associated with infertility. Examples include:
- Cyclophosphamide
- Ifosfamide
- Busulfan
- Chlorambucil
- Platinum-Based Agents: These can also have a significant impact on male fertility. Examples include:
- Cisplatin
- Carboplatin
- Oxaliplatin
- Antimetabolites: Some of these drugs can affect sperm production and quality. Examples include:
- Methotrexate
- 6-mercaptopurine
- Vinca Alkaloids: These drugs can disrupt mitotic spindle formation and affect sperm production. Examples include:
- Vincristine
- Vinblastine
- Taxanes: These drugs can also impact spermatogenesis. Examples include:
- Paclitaxel
- Docetaxel
- Anthracyclines: While less commonly associated with infertility compared to other agents, they can still have an effect. Examples include:
- Doxorubicin
- Epirubicin
Is chemotherapy induced male infertility reversible?
The reversibility of chemotherapy-induced male infertility depends on several factors, including the type and dose of chemotherapy drugs used, the duration of treatment, and individual patient characteristics. Here’s a general overview:
- Type and Dosage of Drugs: Infertility is more likely to be reversible with less toxic agents or lower doses. For example, some patients treated with less aggressive regimens might regain fertility over time.
- Duration of Treatment: Shorter courses of chemotherapy might result in a higher chance of recovery compared to long-term or multiple cycles of treatment.
- Age and Overall Health: Younger men and those in better overall health may have a better chance of regaining fertility after treatment.
- Sperm Production Recovery: Spermatogenesis typically takes about 2-3 months to produce new sperm. It can take several months to years for sperm production to return to normal levels after completing chemotherapy, if it does at all.
- Individual Variation: Recovery can be highly individual. Some men may experience partial recovery of sperm production, while others might have persistent infertility.
Is prevention against chemotherapy induced male infertility possible?
Yes, prevention and mitigation strategies for chemotherapy-induced male infertility are possible. Here are several approaches:
- Fertility Preservation:
- Sperm Banking: Men can store sperm samples before starting chemotherapy. This is one of the most effective methods for preserving fertility.
- Testicular Sperm Extraction (TESE): In cases where sperm banking is not feasible before treatment, sperm can sometimes be retrieved from the testes post-treatment.
- Cryopreservation:
- Gonadal Tissue Cryopreservation: For prepubescent boys or those who cannot provide a sperm sample, cryopreservation of testicular tissue might be considered.
- Pharmacological Interventions:
- Gonadoprotective Agents: Research is ongoing into drugs that might protect the testes from the effects of chemotherapy. For example, agents that reduce oxidative stress or prevent apoptosis in spermatogenic cells could offer protective benefits.
- Adjusting Treatment Protocols:
- Use of Less Gonadotoxic Agents: Oncologists might choose chemotherapy regimens that are less likely to impact fertility, if possible, based on the patient’s specific cancer and overall health.
- Timing and Dosage Adjustments:
- Dose Reductions and Treatment Breaks: In some cases, adjusting the dose or scheduling breaks in chemotherapy might reduce its impact on fertility.
- Hormonal Support:
- Testosterone Replacement Therapy: While not a preventative measure per se, testosterone therapy can help manage symptoms of hormonal imbalance that might result from chemotherapy, though it does not restore fertility.
Diagnosis of chemotherapy induced male infertility
Diagnosing chemotherapy-induced male infertility involves a combination of clinical evaluation, medical history review, and laboratory tests. Here’s a step-by-step approach:
- Medical History and Clinical Evaluation:
- Review Cancer Treatment History
- Assess Symptoms
- Semen Analysis:
- Sperm Count
- Sperm Motility
- Sperm Morphology
- Semen Volume and pH
- Hormonal Profile:
- Testosterone Levels
- Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH)
- Genetic Testing:
- Karyotyping
- Y Chromosome Microdeletions
- Testicular Biopsy:
- Histological Examination: In some cases, a testicular biopsy may be performed to assess sperm production and testicular tissue health.
- Ultrasound Imaging:
- Scrotal Ultrasound: Imaging to identify structural abnormalities or issues in the testes and surrounding areas.
- Consultation with a Specialist:
- Reproductive Endocrinologist: A specialist in male reproductive health can provide a comprehensive evaluation and recommend appropriate treatment or management options.
Treatment of male infertility secondary to chemotherapy
Treating chemotherapy-induced male infertility involves a combination of strategies aimed at managing the effects of chemotherapy on fertility and exploring options for future reproduction. The approach depends on the severity of infertility and individual patient circumstances. Here are common treatments and management strategies:
- Fertility Preservation and Assisted Reproductive Technologies (ART):
- Sperm Banking: Before starting chemotherapy, patients can store sperm for future use. This is the most direct method for preserving fertility.
- In Vitro Fertilization (IVF): If sperm quality is reduced but sperm banking was done, IVF can be used to facilitate conception.
- Intracytoplasmic Sperm Injection (ICSI): For cases with severely reduced sperm count or motility, ICSI involves injecting a single sperm directly into an egg.
- Hormonal Therapy:
- Testosterone Replacement Therapy: While not a fertility restoration treatment, it can manage symptoms related to low testosterone levels resulting from chemotherapy. It does not restore fertility but can improve overall quality of life.
- Medications and Supplements:
- Antioxidants: Supplements like vitamin C, vitamin E, and coenzyme Q10 may help reduce oxidative stress and improve sperm quality.
- Gonadotropin Therapy: In some cases, medications that stimulate the testes to produce sperm may be considered, though their effectiveness can vary.
- Reconstructive Surgery:
- Testicular Sperm Extraction (TESE): If sperm production is severely impaired but viable sperm can be retrieved from the testes, TESE can be used in conjunction with ART techniques.
- Recovery Time:
- Natural Recovery: In some cases, sperm production may gradually return to normal after chemotherapy ends, though this can take months or years. Regular follow-up and semen analysis can monitor recovery.
- Psychological and Emotional Support:
- Counseling: Support from a mental health professional or fertility counselor can help individuals and couples cope with the emotional aspects of infertility and treatment options.
- Future Planning:
- Alternative Family Building Options: For those with persistent infertility, options such as donor sperm or adoption may be considered.
Prognosis of chemotherapy induced male infertility
The prognosis for treatment of chemotherapy-induced male infertility varies widely depending on several factors, including the type and intensity of chemotherapy, the individual’s age and overall health, and the specific treatment interventions used. Here’s an overview of the prognosis based on different aspects:
- Fertility Preservation:
- Sperm Banking: If sperm banking is performed before chemotherapy, the prognosis for future fertility is generally good. Stored sperm can be used for assisted reproductive technologies (ART) such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
- Natural Recovery:
- Spermatogenesis Resumption: Some men may experience a gradual return of sperm production after completing chemotherapy. The timeline for recovery can range from several months to a few years, and the extent of recovery varies. Regular monitoring through semen analysis can help track progress.
- Hormonal and Pharmacological Interventions:
- Effectiveness: Medications and hormone therapies aimed at restoring sperm production or improving sperm quality may have limited success and are not guaranteed to restore fertility. Their effectiveness often depends on the extent of testicular damage.
- Assisted Reproductive Technologies (ART):
- IVF and ICSI: These methods can offer a good chance of successful conception if sperm quality is preserved or if viable sperm can be retrieved. The success rate for ART depends on sperm quality, egg quality, and other factors related to both partners.
- Testicular Sperm Extraction (TESE):
- Outcomes: TESE can be effective for retrieving sperm from the testes even when sperm count is very low or absent in ejaculate. Success rates vary, and the quality of retrieved sperm can impact ART outcomes.
- Long-Term Prognosis:
- Persistent Infertility: Some men may experience permanent infertility due to significant damage from chemotherapy. In such cases, alternative family-building options such as sperm donation or adoption may be considered.
Summary
Chemotherapy-induced male infertility occurs when chemotherapy drugs impair sperm production and quality. This is due to the drugs’ effects on rapidly dividing spermatogenic cells, hormonal imbalances, oxidative stress, and testicular toxicity. Diagnosis typically involves semen analysis, hormonal assessments, and possibly genetic testing. Treatment options include sperm banking before chemotherapy, hormonal therapies, and assisted reproductive technologies such as IVF and ICSI. Recovery of fertility may occur over time for some men, but others may face persistent infertility. A multidisciplinary approach is essential for managing and mitigating the effects of chemotherapy on fertility.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply