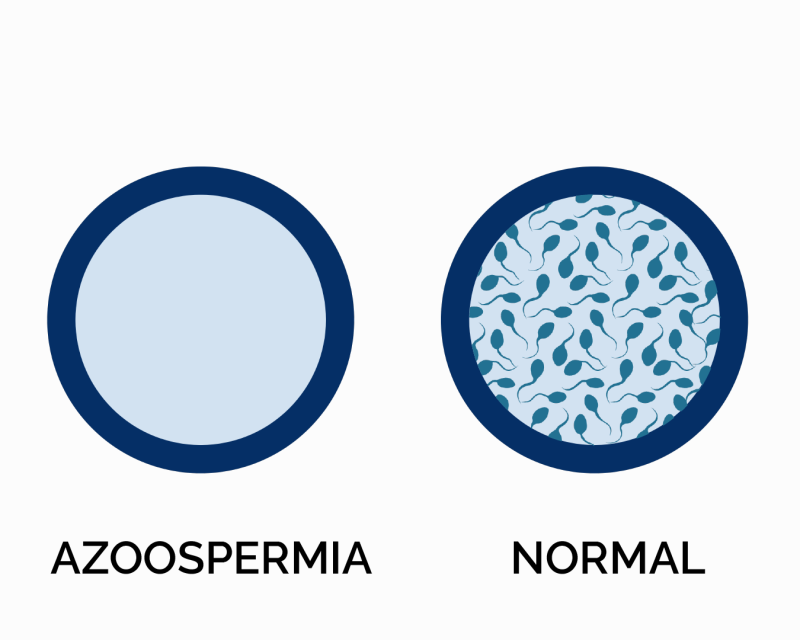
Azoospermia is a medical condition characterized by the complete absence of sperm in a man’s semen. This condition can be a significant factor in male infertility, as sperm is essential for natural conception. Azoospermia can result from various causes, including blockages in the reproductive tract, hormonal imbalances, or genetic issues. Diagnosis typically involves semen analysis, and treatment options may vary depending on the underlying cause, ranging from surgical procedures to assisted reproductive technologies.
What is azoospermia?
Azoospermia is a condition where no sperm are present in a man’s semen (seminal fluid). It is a significant cause of male infertility, as sperm is essential for fertilization. There are two main types of azoospermia:
- Obstructive Azoospermia: Caused by a blockage in the reproductive tract that prevents sperm from being ejaculated. This can result from conditions such as infections, surgeries, or congenital abnormalities.
- Non-Obstructive Azoospermia: Due to a problem with sperm production in the testicles, which can be caused by genetic disorders, hormonal imbalances, or other health issues.
What are the causes of azoospermia?
Azoospermia can arise from various causes, which are typically categorized into two main groups:
Obstructive Azoospermia (post testicular):
This type occurs when there is a blockage in the reproductive tract that prevents sperm from being included in the semen. Causes can include:
- Congenital Absence of the Vas Deferens: A genetic condition where the tubes that transport sperm from the testicles are absent.
- Infections: Such as epididymitis or prostatitis, which can cause scarring or blockage.
- Surgeries: Previous surgeries such as vasectomy or hernia repair that may lead to blockages.
- Trauma: Injury to the reproductive tract.
Non-Obstructive Azoospermia (pre and testicular causes):
This type results from a failure in sperm production or maturation in the testicles. Causes can include:
- Genetic Disorders: Conditions such as Klinefelter syndrome or Y chromosome microdeletions that affect sperm production.
- Hormonal Imbalances: Issues with hormones that regulate sperm production, such as low levels of testosterone or problems with the pituitary gland.
- Testicular Damage: Damage due to conditions like varicocele, radiation, or chemotherapy.
- Chronic Health Conditions: Such as diabetes or kidney disease that can impact sperm production.
Diagnosis
Diagnosing azoospermia involves a series of steps to determine whether sperm are absent from the semen and to identify the underlying cause. Here’s an overview of the diagnostic process:
Semen Analysis:
- Initial Test: The primary test for diagnosing azoospermia is a semen analysis, where a sample of semen is examined under a microscope to check for the presence of sperm.
- Repeat Analysis: Often, multiple samples are tested to confirm the absence of sperm and rule out temporary factors that could affect sperm count.
Medical History and Physical Examination:
- Medical History: Discussing the patient’s medical history, including any previous surgeries, infections, or chronic health conditions.
- Physical Examination: A physical examination to check for any visible signs of reproductive tract issues, such as varicocele or scarring.
Hormonal Testing:
- Blood Tests: Measuring levels of hormones such as testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) to assess if hormonal imbalances are affecting sperm production.
Genetic Testing:
- Karyotyping: To detect chromosomal abnormalities like Klinefelter syndrome.
- Y Chromosome Microdeletions: Testing for deletions in the Y chromosome, which can affect sperm production.
Imaging Studies:
- Ultrasound: An ultrasound of the scrotum and reproductive organs can help identify structural abnormalities or blockages.
Specialized Tests:
- Testicular Biopsy: A biopsy may be performed to assess sperm production within the testicles and determine if sperm are present but not reaching the ejaculate.
Genetic and Infectious Disease Screening:
- Genetic Screening: Additional tests may be conducted for specific genetic conditions that impact sperm production.
- Infectious Disease Testing: To rule out infections that may cause obstruction or affect sperm production.
Treatment
The treatment for azoospermia depends on the underlying cause of the condition. Here’s an overview of potential treatment options for both obstructive and non-obstructive azoospermia:
Obstructive Azoospermia:
When the absence of sperm is due to a blockage or obstruction in the reproductive tract, treatment options may include:
- Surgical Correction: Procedures such as vasovasostomy (vasectomy reversal) or epididymovasostomy can be performed to remove blockages and restore the flow of sperm.
- Transurethral Resection of Ejaculatory Ducts (TURED): If there is a blockage in the ejaculatory ducts, this procedure can help clear the obstruction.
- Sperm Retrieval: In cases where surgical correction is not possible, sperm may be directly retrieved from the testicles or epididymis through techniques like percutaneous epididymal sperm aspiration (PESA) or testicular sperm extraction (TESE) for use in assisted reproductive technologies (ART).
Non-Obstructive Azoospermia:
When azoospermia is caused by issues with sperm production, treatment options vary based on the underlying cause:
- Hormonal Therapy: If hormonal imbalances are detected, medications such as human chorionic gonadotropin (hCG) or follicle-stimulating hormone (FSH) may be prescribed to stimulate sperm production.
- Genetic Counseling: For genetic conditions like Klinefelter syndrome, genetic counseling may help manage expectations and guide decisions about treatment.
- Assisted Reproductive Technologies (ART): Techniques like intracytoplasmic sperm injection (ICSI) can be used to fertilize eggs with sperm retrieved directly from the testicles.
- Lifestyle and Health Management: Addressing underlying health conditions, improving lifestyle factors (such as diet, exercise, and avoiding toxins), and managing chronic conditions can sometimes improve sperm production.
General Approaches:
- Counseling and Support: Psychological support and counseling may be beneficial, especially for individuals coping with infertility and its emotional impact.
- Experimental Treatments: In some cases, newer or experimental treatments may be considered, but these should be discussed with a specialist.
A personalized treatment plan is usually developed in consultation with a urologist or fertility specialist, based on the specific diagnosis and individual circumstances.
Summary
Azoospermia is a condition where there is no sperm present in a man’s semen, leading to infertility. It is categorized into two types: obstructive and non-obstructive. Diagnosis involves semen analysis, hormone tests, genetic screening, and sometimes imaging or biopsy. Treatment depends on the underlying cause.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply