A cystocele, also known as a prolapsed bladder, occurs when the supportive tissue between a woman’s bladder and vaginal wall weakens and stretches, causing the bladder to bulge into the vagina. This condition can result from childbirth, heavy lifting, or straining during bowel movements, and is more common as women age.
Symptoms may include a feeling of fullness or pressure in the pelvis and vagina, discomfort or pain during sex, and urinary problems like incontinence or difficulty emptying the bladder. Treatment options vary depending on severity and can include pelvic floor exercises, a pessary device, or surgery.
What is “cystocele?”
A cystocele, also known as a prolapsed bladder, is a medical condition where the bladder drops from its normal position and bulges into the vaginal wall. This happens due to the weakening of the supportive tissues between the bladder and the vagina, often as a result of childbirth, chronic constipation, heavy lifting, or other activities that put strain on the pelvic floor.
Causes
Cystocele, or bladder prolapse, is caused by the weakening or stretching of the supportive tissues between the bladder and the vaginal wall. Several factors can contribute to this weakening, including:
- Childbirth: Vaginal delivery, especially multiple or difficult deliveries, can stretch and weaken the pelvic floor muscles and supportive tissues.
- Aging and Menopause: As women age and go through menopause, levels of estrogen (a hormone that helps keep the pelvic muscles strong) decrease, leading to weaker tissues.
- Chronic Straining: Activities that cause prolonged straining can put excessive pressure on the pelvic floor, including:
- Chronic constipation and straining during bowel movements
- Heavy lifting
- Persistent coughing (such as from chronic bronchitis or smoking)
- Obesity: Excess body weight increases pressure on the pelvic floor, contributing to tissue weakening.
- Hysterectomy: Removal of the uterus can sometimes affect the support structures of the pelvic organs, leading to prolapse.
- Genetics: A family history of pelvic organ prolapse may increase the risk, suggesting a genetic predisposition to weaker connective tissues.
- Connective Tissue Disorders: Conditions that affect the connective tissues, such as Ehlers-Danlos syndrome, can increase the risk of developing a cystocele.
Risk factors
The risk factors for developing a cystocele (bladder prolapse) include:
- Childbirth: Vaginal deliveries, especially multiple or difficult ones, can stretch and weaken the pelvic floor muscles and supportive tissues.
- Aging: The risk of cystocele increases with age, as the tissues naturally lose strength and elasticity over time.
- Menopause: Decreased estrogen levels after menopause can weaken the pelvic tissues.
- Chronic Straining: Activities that cause prolonged straining, such as:
- Chronic constipation and straining during bowel movements
- Heavy lifting
- Persistent coughing (such as from chronic bronchitis or smoking)
- Obesity: Excess body weight puts additional pressure on the pelvic floor, leading to tissue weakening.
- Hysterectomy: Removal of the uterus can sometimes affect the support structures of the pelvic organs, leading to prolapse.
- Genetic Factors: A family history of pelvic organ prolapse may indicate a genetic predisposition to weaker connective tissues.
- Connective Tissue Disorders: Conditions like Ehlers-Danlos syndrome, which affect connective tissues, can increase the risk of cystocele.
- Previous Pelvic Surgery: Surgeries in the pelvic area can weaken the support structures, increasing the risk of prolapse.
- High-impact Activities: Long-term participation in activities that put repetitive strain on the pelvic floor, such as certain sports, may increase the risk.
Symptoms of cystocele
The symptoms of a cystocele (bladder prolapse) can vary depending on the severity of the condition. Common symptoms include:
- Pelvic Pressure or Fullness: A feeling of pressure, fullness, or heaviness in the pelvic or vaginal area.
- Bulge in the Vagina: A noticeable bulge or protrusion in the vagina, which may be felt or seen, especially when bearing down or straining.
- Urinary Problems:
- Difficulty starting to urinate
- Frequent urination
- Incomplete emptying of the bladder
- Stress incontinence (leakage of urine during activities that increase abdominal pressure, such as coughing, sneezing, or lifting)
- Urgency to urinate
- Discomfort or Pain:
- Discomfort or pain in the pelvic region
- Pain during sexual intercourse
- Recurrent Urinary Tract Infections (UTIs): Frequent UTIs due to incomplete emptying of the bladder.
- Vaginal Bleeding or Discharge: In some cases, there may be abnormal vaginal bleeding or discharge.
- Lower Back Pain: Some women may experience lower back pain.
Diagnosis of cystocele
The diagnosis of a cystocele involves several steps, including taking a medical history, performing a physical examination, and sometimes conducting additional tests. Here is a detailed process for diagnosing a cystocele:
Medical History
- Symptom Inquiry: The healthcare provider will ask about the patient’s symptoms, their duration, and how they impact daily activities.
- Risk Factors: The discussion will include childbirth history, menopause status, any history of pelvic surgeries, chronic constipation, chronic coughing, or heavy lifting.
- Medical Conditions: Review of other medical conditions or family history that might predispose the patient to connective tissue disorders.
Physical Examination
- Pelvic Exam: The doctor will perform a pelvic examination to assess the degree of bladder prolapse. The patient may be asked to bear down (as if straining) to observe the extent of the prolapse.
- Vaginal Speculum: A speculum might be used to get a better view of the vaginal walls and to identify any bulging of the bladder into the vagina.
- Pelvic Floor Muscle Assessment: Evaluation of the strength and function of the pelvic floor muscles.
Additional Tests
- Urinalysis: To check for urinary tract infections or other abnormalities in the urine.
- Postvoid Residual Measurement: An ultrasound or catheter is used to measure the amount of urine left in the bladder after urination.
- Urodynamic Testing: Tests to assess how well the bladder and urethra are storing and releasing urine.
- Pelvic Ultrasound or MRI: Imaging tests to get a detailed view of the pelvic organs and to rule out other conditions.
- Cystourethroscopy: A procedure using a thin, flexible tube with a camera to visually examine the inside of the bladder and urethra.
Grading of cystocele
The severity of the cystocele is often graded based on the extent of the prolapse:
- Stage 1: Mild prolapse where the bladder drops only slightly into the vagina.
- Stage 2: Moderate prolapse where the bladder drops to the opening of the vagina.
- Stage 3: Severe prolapse where the bladder bulges out of the vaginal opening.
- Stage 4: Complete prolapse where the entire bladder protrudes out of the vaginal opening.
Treatment of cystocele
The treatment of a cystocele (bladder prolapse) depends on the severity of the condition, the patient’s symptoms, and overall health. Here are the main treatment options:
Conservative Treatments
Lifestyle Changes
- Weight Management: Maintaining a healthy weight can reduce pressure on the pelvic floor.
- Avoid Heavy Lifting: Reducing activities that strain the pelvic floor can help prevent worsening of the prolapse.
- Manage Constipation: Increasing fiber intake and staying hydrated to avoid straining during bowel movements.
Pelvic Floor Exercises
- Kegel Exercises: Strengthening the pelvic floor muscles can help support the bladder and improve symptoms. These exercises involve repeatedly contracting and relaxing the pelvic floor muscles.
Vaginal Pessary
- Pessary Device: A removable device inserted into the vagina to support the bladder and hold it in place. This is a non-surgical option suitable for many women, especially those who want to avoid surgery or are not surgical candidates.
Medical Treatments
Estrogen Therapy
- Topical Estrogen: Applying estrogen cream, tablet, or ring to the vaginal area can help strengthen and rejuvenate the tissues of the vagina and pelvic floor, particularly in postmenopausal women.
Surgical Treatments
When conservative treatments are not effective, or the cystocele is severe, surgery may be necessary.
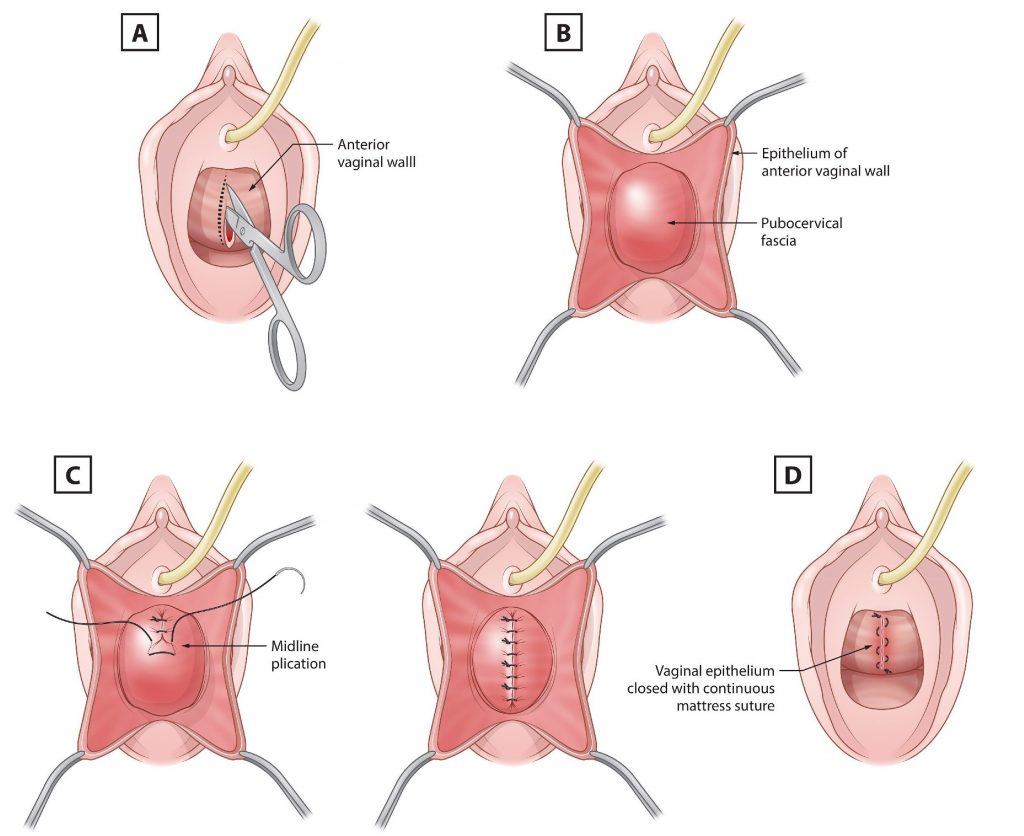
Anterior Colporrhaphy
- Bladder Repair Surgery: The most common surgical procedure for a cystocele. The surgeon makes an incision in the vaginal wall to access the bladder and uses stitches to tighten the tissue and provide additional support.
Vaginal Mesh
- Mesh Implant: In some cases, surgical mesh may be used to reinforce the vaginal wall and support the bladder. However, this option has been associated with complications in some women, and its use has become more controversial.
Hysterectomy
- Uterus Removal: If the patient also has a uterine prolapse or other pelvic organ prolapse, a hysterectomy may be performed in conjunction with the bladder repair.
Postoperative Care
- Pelvic Floor Rehabilitation: Post-surgery physical therapy to strengthen the pelvic floor and prevent recurrence.
- Follow-up Visits: Regular check-ups to monitor healing and ensure the prolapse does not recur.
Summary
A cystocele, or prolapsed bladder, occurs when the supportive tissue between a woman’s bladder and vaginal wall weakens and stretches, causing the bladder to bulge into the vagina. This condition is often caused by childbirth, aging, menopause, chronic straining, or heavy lifting. Symptoms include pelvic pressure, urinary problems, and discomfort during sexual intercourse.
Diagnosis involves a medical history, physical examination, and sometimes additional tests like urinalysis or pelvic imaging. Treatment options range from conservative methods like pelvic floor exercises and pessary devices to surgical interventions, depending on the severity of the prolapse and the patient’s overall health.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply