Peyronie’s disease (PD) is not just a localized condition affecting the penis—it is often linked to systemic diseases involving fibrosis, vascular issues, metabolic disorders, and autoimmune conditions. Research suggests that men with PD are more likely to have conditions such as Dupuytren’s contracture, diabetes, cardiovascular disease, and erectile dysfunction. Understanding these associations can help in early detection, better management, and addressing underlying health risks.
Is PD a presentation of a systemic disease or a local disease?
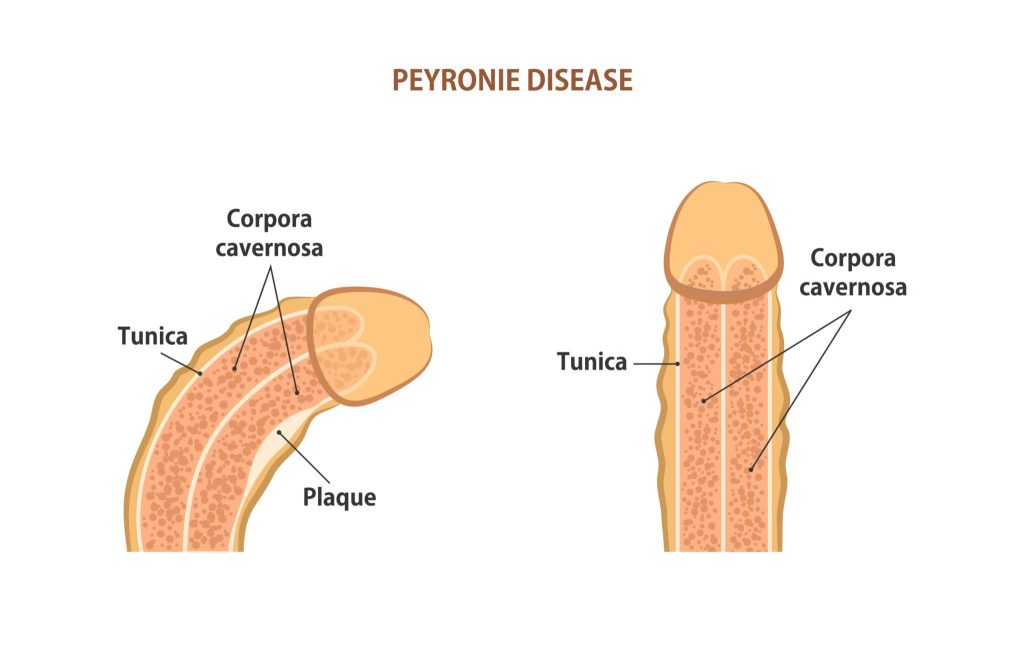
PD is primarily a localized disease affecting the penis, characterized by fibrotic plaque formation in the tunica albuginea. However, research suggests that PD may also be a manifestation of systemic conditions, particularly those involving fibrosis, vascular dysfunction, and metabolic disorders.
Arguments for PD as a local disease:
- It involves localized fibrosis and inflammation in the tunica albuginea.
- Trauma or micro-injury to the penis during intercourse is a common trigger.
- Treatments often target the penis directly (e.g., Xiaflex injections, traction therapy, surgery).
Arguments for PD as a systemic disease presentation:
- PD is associated with fibrotic disorders like Dupuytren’s contracture and Ledderhose disease, suggesting a generalized tendency for fibrosis.
- It is linked to cardiovascular diseases, diabetes, and metabolic syndrome, which involve systemic vascular dysfunction and chronic inflammation.
- Autoimmune and hormonal factors may contribute, indicating a broader systemic involvement.
Conclusion: PD is primarily a localized disease, but in many cases, it reflects underlying systemic conditions like fibrotic disorders, vascular disease, or metabolic dysfunction. Patients with PD should be evaluated for associated systemic health risks to ensure comprehensive management.
Common diseases & conditions associated with PD
PD is linked to several other medical conditions, particularly those involving connective tissue disorders, vascular issues, and metabolic diseases. Here are some of the most common associations:
Connective tissue & fibrotic disorders
PD is characterized by fibrosis (scar tissue formation), making it more common in individuals with other fibrotic conditions:
- Dupuytren’s Contracture → A hand condition where thickened tissue forms in the palm, causing finger contractures. Up to 30% of PD patients also have Dupuytren’s.
- Ledderhose Disease → Fibrosis in the plantar fascia (foot).
- Frozen Shoulder (Adhesive Capsulitis) → A stiffened shoulder due to excessive fibrotic tissue.
Cardiovascular & metabolic diseases
Since PD is linked to vascular inflammation and microvascular damage, it’s often associated with:
- Diabetes Mellitus → Increases the risk of PD due to poor blood flow, nerve damage, and increased fibrosis.
- Hypertension (High Blood Pressure) → Chronic vascular damage may contribute to PD development.
- Atherosclerosis (Plaque Build-up in Arteries) → Poor circulation may impair tissue healing and promote fibrosis.
- Hyperlipidemia (High Cholesterol) → Linked to endothelial dysfunction, which may increase the risk of PD.
- Obesity & Metabolic Syndrome → Inflammation and hormonal imbalances (like low testosterone) can contribute.
Erectile Dysfunction (ED) & urologic conditions
- Veno-Occlusive ED → PD can cause or worsen ED by affecting vascular integrity in the penis.
- Benign Prostatic Hyperplasia (BPH) → Some studies suggest a higher prevalence of PD in men with enlarged prostates.
- Prostate Cancer Treatment → Radical prostatectomy (surgical removal of the prostate) can lead to PD due to nerve damage and scarring.
Autoimmune & Systemic Disorders
PD may have an autoimmune component, linking it to:
- Lupus (SLE) → Chronic inflammation can promote fibrosis.
- Sjögren’s Syndrome → Autoimmune attack on connective tissues may contribute to fibrotic changes.
- Systemic Sclerosis (Scleroderma) → A disease that leads to widespread fibrosis, including in penile tissue.
Hormonal & Endocrine Disorders
- Testosterone Deficiency (Hypogonadism) → Low testosterone may impair tissue repair and increase fibrotic risk.
- Thyroid Disorders (Hypothyroidism, Hyperthyroidism) → Hormonal imbalances can affect connective tissue health.
Neurological Conditions
- Parkinson’s Disease → Some studies suggest a possible link due to neuroinflammatory effects.
- Multiple Sclerosis (MS) → May contribute indirectly by affecting nerve function and erectile health.
Key takeaways: Peyronie’s disease is not just a localized penile condition—it’s often linked to systemic diseases, particularly those involving fibrosis, vascular issues, and metabolic dysfunction. If you have PD, it’s a good idea to check for underlying risk factors like diabetes, cardiovascular disease, or hormonal imbalances.
Why is PD associated with some diseases?
PD is associated with certain diseases due to shared underlying mechanisms such as fibrosis, vascular dysfunction, inflammation, and metabolic imbalances. Here’s why PD is linked to specific conditions:
Fibrosis & connective tissue disorders
- Shared Fibrotic Mechanisms → PD involves excessive collagen deposition and scar formation, similar to conditions like Dupuytren’s contracture and Ledderhose disease.
- Genetic Predisposition → Some individuals may have a genetic tendency toward abnormal connective tissue remodeling, increasing the risk of both PD and fibrotic disorders.
Vascular & cardiovascular diseases
- Microvascular Dysfunction → PD is linked to hypertension, atherosclerosis, and diabetes, which can cause poor blood flow and impair healing.
- Chronic Endothelial Damage → Conditions like heart disease and high cholesterol contribute to endothelial dysfunction, which may trigger fibrosis in penile tissue.
Metabolic disorders (diabetes, obesity, metabolic syndrome)
- Inflammation & Oxidative Stress → High blood sugar and insulin resistance lead to chronic inflammation, increasing the risk of PD.
- Impaired Wound Healing → Diabetes affects collagen metabolism and tissue repair, promoting fibrotic plaque formation in PD.
Hormonal ımbalances
- Low Testosterone (Hypogonadism) → Testosterone plays a role in collagen regulation and tissue repair. Deficiency may contribute to fibrosis and erectile dysfunction.
- Thyroid Disorders → Thyroid hormones influence connective tissue metabolism, potentially affecting PD development.
5Autoimmune & systemic ınflammatory diseases
- Immune Dysregulation → Conditions like lupus, Sjögren’s syndrome, and scleroderma involve chronic inflammation and abnormal connective tissue changes, similar to PD.
ED & neurological conditions
- Venous Leak & Penile Trauma → ED and PD share vascular risk factors, and ED can lead to repetitive microtrauma, increasing PD risk.
- Neurological Diseases (e.g., Parkinson’s, MS) → Nerve dysfunction may contribute to vascular and fibrotic changes seen in PD.
Conclusion: Peyronie’s disease is linked to various conditions due to common pathways of fibrosis, inflammation, vascular dysfunction, and metabolic imbalances. Identifying these associations can help with early detection, better management, and addressing underlying health risks in PD patients.
Summary
PD is commonly associated with fibrotic disorders (e.g., Dupuytren’s contracture), cardiovascular diseases (e.g., hypertension, atherosclerosis), metabolic conditions (e.g., diabetes, obesity), and hormonal imbalances (e.g., low testosterone). It also shares links with autoimmune diseases, neurological disorders, and erectile dysfunction. Identifying and managing these related conditions can improve overall health outcomes for PD patients.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul-TURKIYE


Leave a Reply