Erectile dysfunction (ED) is a common issue among paraplegic patients, resulting from the neurological disruptions caused by spinal cord injuries. This condition can significantly impact quality of life, self-esteem, and intimate relationships. Here i will give information about how spinal cord injuries affect the physiological pathways responsible for ED, current diagnostic approaches, and treatment options available.
Mechanisms of ED paraplegic patients
ED in paraplegic patients is primarily due to disruptions in the nervous system pathways involved in erectile function. Here are the key mechanisms:
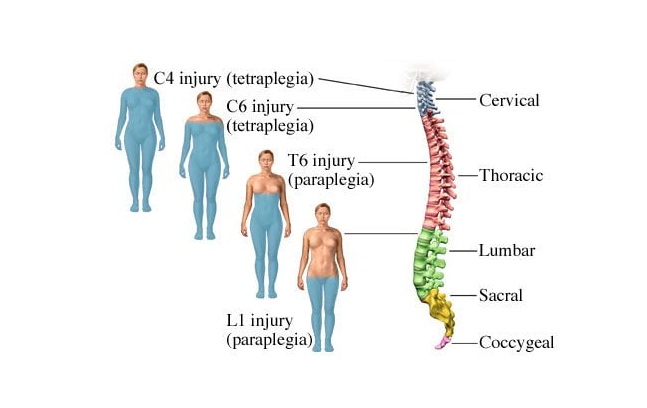
- Neurological Disruption: The spinal cord injury (SCI) interrupts the pathways necessary for the reflexogenic and psychogenic erectile responses. Reflexogenic erections (those triggered by physical stimulation) rely on the sacral spinal cord segments (S2-S4), while psychogenic erections (those triggered by mental or emotional stimulation) are controlled by the thoracolumbar region (T11-L2). Injuries at different levels of the spinal cord can variably impact these mechanisms.
- Reflexogenic vs. Psychogenic Erections:
- Reflexogenic Erections: These are often preserved in patients with injuries above the sacral segments if the sacral cord is intact, enabling some physical response despite other limitations.
- Psychogenic Erections: These are typically compromised in patients with higher-level injuries because the pathways that communicate arousal signals from the brain are interrupted.
- Autonomic Nervous System Dysfunction: SCI affects the autonomic nervous system, which plays a vital role in erectile function through sympathetic and parasympathetic control. Damage to the sympathetic nerves (T11-L2) reduces the ability to initiate and maintain erections, while disruption to the parasympathetic nerves (S2-S4) may impair erectile firmness.
- Vascular Changes: Reduced blood flow or vascular health changes are common following SCI, further compromising erectile function. Blood flow to the penile tissues is critical for achieving and maintaining an erection, and SCI can diminish this through both direct neurological impairment and secondary physical health changes.
- Hormonal Factors: Some SCI patients may experience hormonal imbalances, including lowered testosterone levels, which can impact libido and erectile function.
Diagnosis of ED in paraplegic patients
Diagnosing ED in paraplegic patients involves a combination of medical history assessment, physical exams, neurological evaluations, and specialized diagnostic tests to determine the severity and underlying causes of ED. Here’s an outline of the key diagnostic steps:
- Medical history: The clinician reviews the patient’s injury level, type of spinal cord injury (SCI), onset, and duration. Other factors, such as medications, lifestyle, and psychological well-being, are also assessed, as they can contribute to ED.
- Physical Examination: A physical exam helps assess any physical abnormalities, muscle tone, and reflexes. Examination of the sacral area is particularly important to understand potential damage to the sacral reflexogenic centers involved in erection.
- Neurological Assessment: Neurological exams identify the level and completeness of the SCI, which helps predict erectile capacity (reflexogenic vs. psychogenic erections) based on the injury’s impact on specific spinal pathways.
- Reflexogenic Erection Testing: The bulbocavernosus reflex test is often performed to assess reflexogenic erections. When the glans penis is squeezed, a contraction in the anal sphincter confirms an intact reflex arc, suggesting that reflexogenic erections might be possible if the sacral cord is preserved.
- Vascular and Penile Doppler Ultrasound: A penile Doppler ultrasound can assess blood flow and vascular health in the penile tissue. This helps determine if there are any vascular issues contributing to ED, as reduced blood flow is common in SCI patients.
- Nocturnal Penile Tumescence (NPT) Testing: NPT testing evaluates the presence and quality of erections during sleep, helping differentiate between physical and psychological causes. In paraplegic patients, the absence of nocturnal erections may confirm a neurological basis for ED.
- Pharmacologic Testing: Intracavernosal injections of vasodilators (e.g., alprostadil) can induce an erection, allowing assessment of erectile response. This helps differentiate between neurogenic and vascular causes.
- Hormonal Evaluation: Blood tests to measure testosterone, prolactin, and other hormone levels are performed to rule out hormonal deficiencies or imbalances that could be contributing to ED.
- Psychosocial Assessment: Emotional and mental health, relationship factors, and lifestyle are also considered in diagnosis, as psychological factors may worsen ED symptoms and impact treatment.
Treatment of ED in paraplegic patients
Treating erectile dysfunction (ED) in paraplegic patients requires a multifaceted approach tailored to the patient’s level and type of spinal cord injury (SCI) and individual preferences. Here are the primary treatment options:
- Oral Medications: Phosphodiesterase type 5 (PDE5) inhibitors, such as sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra), are first-line therapies. These medications improve blood flow to the penis but may have limited efficacy in some patients with neurological injuries.
- Intracavernosal injections: For patients who don’t respond to oral medications, injections of vasodilators like alprostadil directly into the penile tissue can help achieve an erection. These injections stimulate blood flow and are effective even when other methods fail.
- Intraurethral suppositories: Alprostadil suppositories can be inserted into the urethra, providing an alternative for patients who prefer to avoid injections.
- Vacuum erection devices (VEDs): VEDs create a vacuum around the penis, drawing blood into the penile tissue to produce an erection. A constriction ring is then applied at the base of the penis to maintain the erection. This method is effective and noninvasive.
- Penile implants: For patients who do not respond to pharmacological or other treatments, a surgical penile implant may be an option. Implants can be inflatable or semi-rigid, allowing patients to achieve an erection on demand. This is generally a last-resort option but can provide reliable results for some.
- Testosterone Replacement Therapy (TRT): If low testosterone levels are identified, TRT may help improve libido and erectile function.
- Lifestyle Modifications: Regular exercise, a balanced diet, and quitting smoking can improve overall vascular health, which may positively impact erectile function. Maintaining a healthy weight and managing other conditions like diabetes and hypertension are also beneficial.
- Psychological Counseling: ED can affect relationships, induvidual and couples therapy can provide support and help both partners adjust to the physical and emotional challenges of SCI and ED.
- Regenerative Medicine: Experimental therapies, including stem cell therapy and platelet-rich plasma (PRP) injections, are being researched for their potential to repair damaged nerves and improve erectile function.
- Low-Intensity Extracorporeal Shockwave Therapy (LI-ESWT): This noninvasive therapy uses sound waves to stimulate blood vessel growth, which may improve erectile function in some patients, though more research is needed on its effectiveness for SCI.
Combining these approaches can often yield the best results, as treatment plans must consider the unique physical, neurological, and psychological needs of each paraplegic patient.
Summary
Paraplegic patients often experience ED due to disrupted nerve pathways, altered blood flow, and hormonal imbalances. Diagnosis typically involves medical history, physical and neurological exams, and tests such as Doppler ultrasounds and hormone assessments. Treatment options include medications (PDE5 inhibitors, injections), mechanical aids (vacuum devices, implants), lifestyle modifications, and psychological support.
Emerging therapies, like regenerative medicine, offer future possibilities. A tailored, multi-faceted approach helps address the unique needs of paraplegic patients managing ED.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE



Leave a Reply