Erectile dysfunction secondary to pelvic radiation refers to the condition where an individual experiences difficulties in achieving or maintaining an erection as a result of radiation therapy targeting the pelvic region. This type of erectile dysfunction (ED) is a common side effect for patients undergoing treatment for cancers such as prostate, bladder, or rectal cancer. Radiation can damage the blood vessels and nerves responsible for erectile function, leading to varying degrees of sexual dysfunction. Understanding this condition is crucial for developing effective treatment strategies and improving the quality of life for affected individuals.
Addressing ED in these patients often involves a multidisciplinary approach, including pharmacological interventions, counseling, and lifestyle modifications.
Indications of pelvic radiotherapy
Pelvic radiotherapy is a treatment method used to target and destroy cancerous cells in the pelvic region. It is often used as part of a comprehensive cancer treatment plan. Here are some common indications for pelvic radiotherapy:
- Prostate Cancer
- Bladder Cancer
- Rectal Cancer
- Anal Cancer
- Metastatic Cancer
- Lymphoma
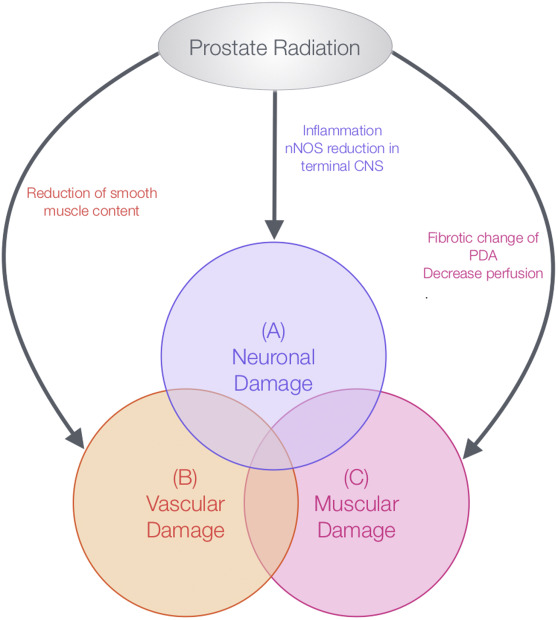
Mechanisms of ED secondary to pelvic radiation
ED secondary to pelvic radiation occurs due to several mechanisms related to the effects of radiation on the pelvic region. Here are the primary mechanisms:
- Vascular Damage: Radiation can cause damage to the blood vessels in the pelvic region, leading to reduced blood flow to the penis. This vascular damage can result in the inability to achieve or maintain an erection, as erections rely on increased blood flow to the penile tissues.
- Nerve Damage: The nerves responsible for erectile function, including the cavernous nerves, can be affected by radiation therapy. Damage to these nerves can impair the signaling pathways necessary for initiating and maintaining an erection.
- Fibrosis and Tissue Changes: Radiation can cause fibrosis, which is the formation of excess fibrous connective tissue, in the erectile tissues. This can lead to stiffness and reduced elasticity, impacting the ability of the penile tissues to expand and fill with blood during an erection.
- Hormonal Changes: Radiation therapy can affect the production and regulation of hormones involved in sexual function, such as testosterone. Hormonal imbalances can contribute to erectile dysfunction and decreased libido.
- Psychological Impact: The stress and emotional burden of undergoing cancer treatment, along with changes in body image and self-esteem, can contribute to psychological factors that exacerbate erectile dysfunction.
- Endothelial Dysfunction: Radiation can impair the function of the endothelium, the inner lining of blood vessels, leading to a reduced ability to produce nitric oxide. Nitric oxide is crucial for the vasodilation required for erections.
- Damage to Adjacent Structures: Radiation can also affect other structures in the pelvic region, such as the bladder and rectum, leading to additional complications that can indirectly impact erectile function.
Diagnosis of ED secondary to pelvic radiation
Diagnosing ED secondary to pelvic radiation involves a comprehensive approach that includes a thorough medical history, physical examination, and various diagnostic tests. Here’s a structured approach to diagnosis:
- Medical History:
- Cancer Treatment History: Review the details of the patient’s cancer diagnosis and treatment, including the type, dose, and duration of pelvic radiation.
- Sexual History: Obtain information about the onset, duration, and severity of erectile dysfunction, as well as any previous sexual function.
- Medical and Psychological History: Assess for other potential causes of ED, including comorbid conditions (e.g., diabetes, cardiovascular disease) and psychological factors (e.g., stress, depression).
- Physical Examination:
- Genital and Pelvic Examination: Evaluate the genitalia and pelvic region for any abnormalities or signs of tissue changes resulting from radiation.
- Vascular and Neurological Assessment: Check for signs of vascular issues (e.g., decreased pulse) and neurological deficits that may affect erectile function.
- Laboratory Tests:
- Hormone Levels: Measure serum testosterone and other relevant hormones to assess for hormonal imbalances that could contribute to ED.
- Blood Glucose and Lipid Profile: Check for conditions like diabetes or dyslipidemia that could exacerbate ED.
- Imaging Studies:
- Ultrasound: Penile Doppler ultrasound can assess blood flow and detect any vascular abnormalities.
- Magnetic Resonance Imaging (MRI): In some cases, MRI may be used to visualize structural changes in the pelvic region or surrounding tissues.
- Specialized Tests:
- Penile Erection Test: Tests such as the nocturnal penile tumescence (NPT) test can evaluate erectile function during sleep, helping to differentiate between physiological and psychological causes of ED.
- Cavernosometry and Cavernosography: These tests measure blood pressure in the penile arteries and assess blood flow and venous leakage.
- Psychological Evaluation:
- Assessment Tools: Use validated questionnaires and scales (e.g., International Index of Erectile Function) to evaluate the psychological and emotional aspects of ED.
- Multidisciplinary Consultation:
- Urologist: Consult with a urologist for expert evaluation and management of erectile dysfunction.
- Oncologist: Discuss the impact of cancer treatment and potential modifications to the treatment plan if necessary.
Symptoms of ED secondary to pelvic radiation
ED secondary to pelvic radiation can present with various symptoms, which may include:
- Difficulty Achieving an Erection: Inability to get an erection sufficient for sexual intercourse, or difficulty starting the erection process.
- Difficulty Maintaining an Erection: Erection may be achieved but cannot be sustained long enough for satisfactory sexual activity.
- Reduced Frequency of Erections: A noticeable decrease in the frequency of spontaneous or morning erections.
- Decreased Sexual Desire: Reduced libido or sexual interest, which may be related to psychological effects or hormonal changes.
- Soft or Flaccid Erections: Erections may be notably softer or less rigid compared to pre-treatment experiences.
- Pain or Discomfort: Some individuals may experience discomfort or pain in the pelvic region or genital area, which can affect erectile function.
- Altered Ejaculation: Changes in the ejaculatory process, including premature ejaculation or delayed ejaculation, can sometimes accompany erectile dysfunction.
- Psychological Symptoms: Anxiety, depression, or distress related to sexual performance or changes in sexual function may be present.
Treatment of ED secondary to pelvic radiation
Treating ED secondary to pelvic radiation involves a combination of medical, psychological, and lifestyle approaches. Here’s a comprehensive overview of potential treatments:
- Pharmacological Treatments:
- Phosphodiesterase Type 5 Inhibitors: Medications such as sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra) can improve blood flow to the penis and help achieve and maintain an erection.
- Intracavernosal Injections: Medications like alprostadil can be injected directly into the penis to induce an erection.
- Intraurethral Therapy: Alprostadil can also be administered as a suppository inserted into the urethra to help stimulate an erection.
- Mechanical Devices:
- Vacuum Erection Devices: These devices create a vacuum around the penis to enhance blood flow and help achieve an erection. A constriction ring is then placed at the base of the penis to maintain the erection.
- Penile Implants:
- Inflatable Implants: These devices consist of inflatable cylinders placed in the penis, a pump in the scrotum, and a reservoir. They allow for control over the timing and firmness of an erection.
- Malleable Implants: These are semi-rigid rods inserted into the penis that can be manually adjusted to achieve an erection.
- Hormone Therapy:
- Testosterone Replacement Therapy: If hormonal imbalances are identified (e.g., low testosterone levels), hormone replacement therapy might be considered to improve sexual function.
- Psychological Counseling:
- Sex Therapy: Counseling with a sex therapist can help address psychological factors contributing to ED, such as anxiety, depression, or relationship issues.
- Cognitive Behavioral Therapy (CBT): CBT can help manage stress, anxiety, and other psychological factors affecting sexual function.
- Lifestyle Modifications:
- Healthy Diet and Exercise: Adopting a balanced diet and regular exercise can improve overall health and potentially enhance erectile function.
- Smoking Cessation and Alcohol Moderation: Reducing or eliminating smoking and excessive alcohol consumption can positively impact erectile function.
- Pelvic Floor Exercises:
- Kegel Exercises: Strengthening the pelvic floor muscles through specific exercises may improve erectile function and overall sexual health.
- Managing Underlying Conditions:
- Control of Chronic Diseases: Proper management of conditions like diabetes, hypertension, and cardiovascular disease can help mitigate their impact on erectile function.
- Surgical Options:
- Vascular Surgery: In some cases, surgical procedures may be considered to address vascular issues contributing to ED, although this is less common for radiation-induced ED.
- Penile ESWT: Extracorporeal Shock Wave Therapy (ESWT) is a non-invasive treatment that uses acoustic waves to stimulate healing and improve blood flow. It’s increasingly used to treat ED, including cases secondary to pelvic radiation.
- Stem cell therapy: Stem cell therapy involves using stem cells to regenerate damaged tissues and restore normal function. In the context of ED secondary to pelvic radiation, stem cell therapy aims to repair the damaged penile tissues and improve erectile function.
- Supplements: Certain supplements containing L-arginine, pycnogenol, panax, icariin etc… may help manage ED secondary to pelvic radiation by supporting overall vascular health, nerve function, and hormonal balance.
- Penile Platelet-Rich Plasma (PRP): Penile PRP therapy offers a potential treatment for ED secondary to pelvic radiation by promoting tissue repair, improving blood flow, and supporting nerve function. While promising, it is essential to work with a urologist to assess suitability and develop a personalized treatment plan.
Prognosis of ED secondary to pelvic radiation
The prognosis of ED secondary to pelvic radiation varies depending on several factors, including the extent of radiation-induced damage, the patient’s overall health, and the effectiveness of treatment interventions. Here’s a general overview:
- Degree of Recovery:
- Early Post-Treatment: ED can be more pronounced shortly after radiation therapy, and some degree of recovery might occur over time. The extent of recovery often depends on the dosage and duration of radiation, as well as individual response.
- Long-Term Outcomes: Some patients may experience partial or complete recovery of erectile function over several months to years, while others may have persistent ED. Long-term prognosis can be influenced by ongoing management strategies and the presence of other health conditions.
- Impact of Treatment:
- Medical Treatments: Many patients respond well to pharmacological treatments (e.g., PDE5 inhibitors) and mechanical devices, which can significantly improve erectile function. The success of these treatments often depends on the severity of the ED and the presence of other underlying conditions.
- Psychological Support: Addressing psychological factors through therapy can improve outcomes and help patients cope with the emotional aspects of ED.
- Role of Rehabilitation:
- Pelvic Floor Exercises: Engaging in pelvic floor exercises may contribute to better outcomes and improved erectile function.
- Lifestyle Modifications: Adopting a healthy lifestyle, including regular exercise, a balanced diet, and smoking cessation, can positively affect erectile function and overall health.
- Individual Variation:
- Patient-Specific Factors: Prognosis can vary based on individual factors such as age, overall health, the presence of comorbid conditions (e.g., diabetes, cardiovascular disease), and the extent of radiation-related tissue damage.
- Multidisciplinary Approach:
- Comprehensive Care: A multidisciplinary approach involving urologists, oncologists, mental health professionals, and other specialists can improve management and outcomes. Tailored treatment plans that address both physical and psychological aspects of ED are often more effective.
Summary
ED secondary to pelvic radiation occurs when radiation therapy, typically used to treat cancers in the pelvic region, leads to difficulties in achieving or maintaining an erection. The condition results from damage to blood vessels, nerves, and surrounding tissues, as well as potential hormonal changes. Symptoms include difficulty achieving or sustaining an erection, reduced frequency of erections, and decreased sexual desire. Diagnosis involves a comprehensive evaluation of medical history, physical examination, and possibly imaging or laboratory tests.
Treatment options include pharmacological therapies, mechanical devices, penile implants, hormone therapy, psychological counseling, and lifestyle modifications. The prognosis varies, with some patients experiencing partial or full recovery over time, particularly with early and effective management.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply