Urethral stricture is a medical condition where the urethra, the tube that carries urine out of the body, becomes narrowed. This narrowing can cause discomfort, difficulty urinating, and other complications. To address this issue, medical procedures like internal urethrotomy and urethroplasty are commonly performed. This FAQ section is designed to provide clear and concise answers to common questions about urethral strictures, the procedures used to treat them, and what patients can expect during recovery.
FAQs for urethral stricture, ınternal urethrotomy, and urethroplasty
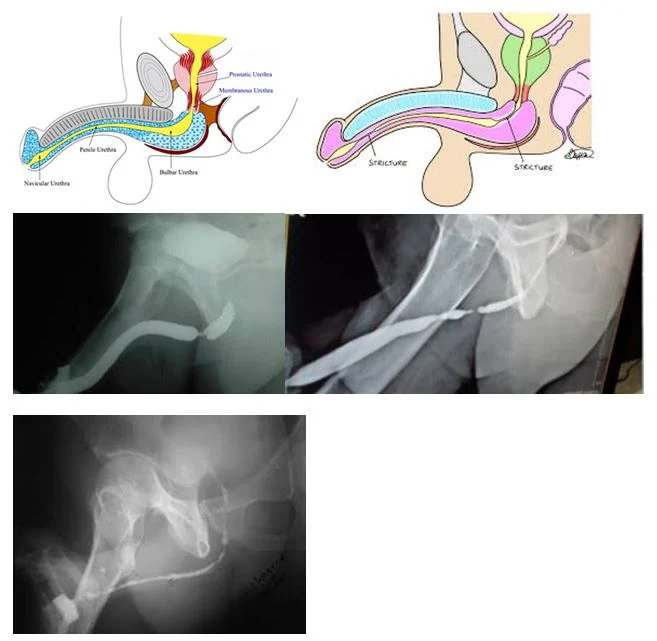
What is a urethral stricture?
A urethral stricture is a narrowing of the urethra, the tube that carries urine from the bladder out of the body. This can lead to difficulty urinating and other urinary problems.
Is female urethral stricture common?
Female urethral stricture is less common than in men. This is primarily due to the shorter length of the female urethra, which is less prone to trauma and scarring. Additionally, females are less likely to have conditions that lead to strictures, such as prostate issues or frequent catheterization.
What causes a urethral stricture?
The causes of urethral stricture include:
- Trauma
- Infection
- Inflammatory Conditions
- Surgery
- Congenital Abnormalities
- Radiation Therapy
- Catheterization
- Previous Treatments
How is a urethral stricture diagnosed?
Diagnosis typically involves a physical examination, urine tests, imaging studies like a retrograde urethrogram, and sometimes cystoscopy, where a camera is inserted into the urethra.
What are the symptoms of urethral strictue?
- Weak urine stream
- Difficulty urinating
- Frequent urination
- Incomplete bladder emptying
- Urinary retention
- Spraying or splitting of the urine stream
- Pain or discomfort
- Recurrent urinary tract ınfections (utıs)
- Blood in the urine (hematuria)
Differential diagnosis of urethral stricture?
- Urethral cancer
- Bladder outlet obstruction (boo)
- Urethral diverticulum
- Pelvic fracture urethral ınjury
- Meatal stenosis
- Neurogenic bladder
- Urinary tract ınfection (utı)
- Prostatitis
What is an internal urethrotomy?
Internal urethrotomy is a minimally invasive procedure where a small incision is made in the stricture to widen the urethra. This is often done using a special instrument called a cystoscope.
What is a urethroplasty?
Urethroplasty is a surgical procedure to repair the urethra. It involves removing the narrowed section of the urethra and reconnecting the healthy ends or using tissue grafts to reconstruct the urethra.
How do I know which treatment is right for me?
The choice between internal urethrotomy and urethroplasty depends on factors like the length and location of the stricture, previous treatments, and overall health. Your urologist will recommend the best option based on your specific situation.
What is the recovery process like for these procedures?
Recovery varies depending on the procedure. Internal urethrotomy usually has a shorter recovery time, while urethroplasty may require a longer healing period. Your doctor will provide detailed post-operative care instructions.
Can urethral strictures recur after treatment?
Yes, urethral strictures can recur, especially after an internal urethrotomy. Urethroplasty generally has a lower recurrence rate, but ongoing monitoring is important.
What are the indications of internal urethrotomy?
- Short Urethral Strictures: It is most effective for treating short strictures, generally less than 1-2 centimeters in length.
- Primary or Recurrent Strictures: Internal urethrotomy can be used for both first-time treatment of a stricture or for recurrent strictures, especially if they recur after previous dilation or surgery.
- Bulbar Urethral Strictures: It is often indicated for strictures located in the bulbar urethra, the section of the urethra located in the perineum.
- Patients Unfit for Major Surgery: Internal urethrotomy is a less invasive option compared to urethroplasty, making it suitable for patients who may not be fit for a more extensive surgical procedure due to age, comorbidities, or other health considerations.
- Failed Conservative Treatments: If less invasive treatments, like urethral dilation, have failed, internal urethrotomy may be indicated as the next step.
- Minimally Invasive Approach: When a minimally invasive procedure is preferred, internal urethrotomy is a good option.
- Patient Preference: Some patients may prefer internal urethrotomy due to the shorter recovery time and the avoidance of more extensive surgery.
What are the indications of open urethroplasty?
- Long Urethral Strictures: It is typically recommended for longer strictures, often greater than 2 centimeters, which are not amenable to less invasive treatments like internal urethrotomy.
- Complex Strictures: Strictures that are complex in nature, including those caused by trauma, infection, or previous surgeries, often require urethroplasty for effective treatment.
- Recurrent Strictures after Other Treatments: If a stricture recurs after internal urethrotomy, dilation, or other minimally invasive procedures, urethroplasty may be indicated as a more definitive solution.
- Panurethral Strictures: For strictures involving the entire length of the urethra (panurethral strictures), open urethroplasty is often the preferred treatment.
- Strictures with Significant Scarring: When there is extensive scarring of the urethra or surrounding tissues, open urethroplasty may be necessary to remove scar tissue and reconstruct the urethra.
- Strictures Associated with Fistulas or Diverticula: Urethroplasty is indicated when strictures are complicated by the presence of urethral fistulas or diverticula, requiring a more complex surgical repair.
- Patients Requiring a Durable, Long-Term Solution: Urethroplasty is often chosen when a long-lasting solution is needed, as it has a lower recurrence rate compared to internal urethrotomy or dilation.
- Failed Previous Urethroplasty: If a previous urethroplasty has failed, a more extensive or revised urethroplasty may be required.
What are the complications of urethral stricture surgery?
- Infection
- Bleeding:
- Urinary Incontinence
- Stricture Recurrence
- Urethral Fistula:
- Erectile Dysfunction
- Delayed Healing
- Pain
- Narrowing or Scarring
Do urethroplasty and internal urethrotomy cause erectile dysfunction and infertility?
Urethroplasty:
- Erectile Dysfunction: Can occur, especially if the surgery involves the bulbar urethra or nearby structures. The risk is higher with extensive procedures or if there is significant disruption to surrounding tissues.
- Infertility: Typically, urethroplasty does not directly affect fertility. However, complications or scarring might potentially impact the ejaculatory process or lead to retrograde ejaculation in some cases, which could indirectly affect fertility.
Internal Urethrotomy:
- Erectile Dysfunction: Generally, the risk is lower compared to urethroplasty due to its less invasive nature. However, there is still a small risk of affecting erectile function if the procedure impacts surrounding tissues.
- Infertility: Similar to urethroplasty, internal urethrotomy is unlikely to directly impact fertility. The primary concerns are related to the potential for scarring or complications that might affect ejaculation or cause retrograde ejaculation.
Summary
This FAQ section addresses common questions about urethral strictures, internal urethrotomy, and urethroplasty. It covers what a urethral stricture is, its causes, symptoms, and diagnosis. It explains internal urethrotomy as a minimally invasive procedure for short or recurrent strictures and outlines its indications. It also provides information on urethroplasty, a more extensive surgical option for long or complex strictures, including its indications and recovery process.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply