Female urethral stricture is a rare but significant condition characterized by the narrowing of the urethra, leading to difficulty in urination. It can result from infections, trauma, previous surgeries, or inflammatory conditions. Common symptoms include weak urine flow, frequent urinary tract infections, and incomplete bladder emptying. Diagnosis involves uroflowmetry, cystoscopy, and imaging tests.
Treatment options range from urethral dilation to more advanced surgical interventions, such as urethroplasty, depending on the severity of the stricture. Early diagnosis and appropriate treatment can improve urinary function and quality of life.
What is female urethral stricture?
Female urethral stricture is a condition where the urethra (the tube that carries urine from the bladder out of the body) becomes abnormally narrowed, leading to difficulties in urination. This narrowing can result from scarring due to infections, trauma, previous surgeries, or chronic inflammation. While rare compared to male urethral strictures, it can cause significant discomfort and complications, such as urinary retention, recurrent urinary tract infections (UTIs), and incomplete bladder emptying. Treatment options range from minimally invasive procedures like urethral dilation to surgical reconstruction, depending on the severity of the stricture.
Causes of female urethral stricture?
Female urethral strictures can develop due to several factors that lead to scarring and narrowing of the urethra. Key causes include:
- Infections: Recurrent or severe urinary tract infections (UTIs) can cause inflammation that eventually leads to scar tissue formation.
- Trauma: Injury to the pelvic region from childbirth, accidents, or other physical trauma can damage the urethra, resulting in scarring.
- Previous Surgeries: Pelvic or urethral surgeries, including procedures that involve catheterization, may inadvertently injure the urethral lining.
- Inflammatory Conditions: Chronic inflammatory diseases, such as lichen sclerosus, can also contribute to the development of strictures by inducing fibrosis in the urethral tissue.
Each of these factors can individually or collectively lead to the narrowing of the urethra, resulting in the symptoms associated with female urethral stricture.
Symptoms of female urethral stricture?
The symptoms of female urethral stricture can vary in severity but typically include:
- Weak or slow urine stream – Difficulty in passing urine or reduced flow.
- Straining to urinate – Needing to push or strain to start or complete urination.
- Frequent urination – Feeling the need to urinate more often than usual.
- Incomplete bladder emptying – A sensation that the bladder is not fully emptied after urination.
- Urinary retention – Inability to completely empty the bladder, leading to discomfort.
- Painful urination (dysuria) – Burning or pain while urinating.
- Recurrent urinary tract infections (UTIs) – Frequent infections due to urine stagnation.
- Dribbling after urination – Leakage or dripping of urine after finishing.
- Pelvic pain or discomfort – Pain in the lower abdomen or pelvic area due to urinary issues.
Diagnosis
Diagnosing female urethral stricture involves a combination of medical history, physical examination, and specialized tests to evaluate urethral narrowing and its impact on urinary function.
1. Medical History and Physical Examination
- Review of symptoms (e.g., weak urine stream, frequent UTIs, difficulty urinating).
- Assessment of previous surgeries, infections, or trauma to the urinary tract.
- Pelvic examination to check for tenderness or abnormalities.
2. Diagnostic Tests
- Uroflowmetry – Measures urine flow rate; a slow or interrupted stream may indicate a stricture.
- Post-void Residual (PVR) Test – Uses ultrasound or catheterization to check for urine left in the bladder after urination.
- Cystourethroscopy – A small camera (cystoscope) is inserted into the urethra to visualize narrowing, scarring, or other abnormalities.
- Retrograde Urethrogram (RUG) or Voiding Cystourethrogram (VCUG) – X-ray imaging with contrast dye to highlight the urethra and bladder while urinating.
- MRI or Pelvic Ultrasound – In some cases, imaging is used to assess surrounding tissues and rule out other conditions.
Complications
If left untreated, female urethral stricture can lead to several complications, including:
1. Urinary Retention
- Difficulty or inability to fully empty the bladder, causing discomfort and an increased risk of infection.
2. Recurrent Urinary Tract Infections (UTIs)
- Stagnant urine in the bladder creates an environment for bacterial growth, leading to frequent infections.
3. Bladder Dysfunction
- Chronic obstruction can weaken the bladder muscle over time, reducing its ability to contract properly.
4. Kidney Damage (Hydronephrosis)
- Severe cases may cause urine to back up into the kidneys, leading to swelling (hydronephrosis) and potential kidney damage.
5. Bladder Stones
- Incomplete emptying of the bladder can lead to stone formation, causing pain and further urinary obstruction.
6. Incontinence
- Straining to urinate or untreated strictures may contribute to urine leakage or overflow incontinence.
7. Chronic Pelvic Pain
- Persistent discomfort or pain in the pelvic region due to prolonged bladder dysfunction.
Treatment of female urethral stricture
The treatment of female urethral stricture depends on the severity of the narrowing, underlying causes, and the patient’s symptoms. Options range from minimally invasive procedures to surgical reconstruction.
Conservative Management
- Catheterization: In some cases, a temporary or intermittent catheter may be used to relieve urinary retention.
- Medications: If associated with infections or inflammation, antibiotics or anti-inflammatory drugs may be prescribed.
Minimally Invasive Procedures
- Urethral Dilation: A procedure where progressively larger dilators or a balloon catheter are used to widen the narrowed urethra. This offers temporary relief but has a high recurrence rate.
- Direct Vision Internal Urethrotomy (DVIU): A small incision is made in the stricture using a cystoscope with a tiny blade or laser. This is often effective for mild strictures but may require repeat procedures.
Surgical treatment (female urethroplasty)
Female urethroplasty is a reconstructive surgical procedure designed to correct urethral strictures that have not responded to less invasive treatments like dilation or internal urethrotomy. The goal of the surgery is to restore a normal urethral caliber and improve urinary function.
Indications:
- Recurrent or persistent strictures unresponsive to conservative management.
- Severe narrowing causing significant urinary symptoms such as retention, recurrent infections, or impaired bladder emptying.
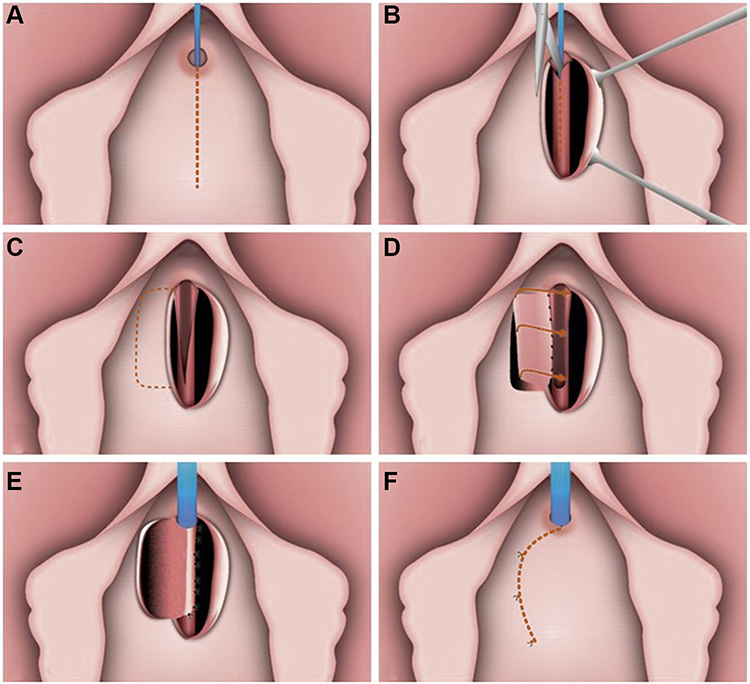
Surgery-urethroplasty
- Excision and Primary Anastomosis: In cases where the stricture is short, the narrowed segment may be excised and the healthy ends of the urethra rejoined.
- Augmentation/Urethroplasty with Flaps or Grafts: For longer or more complex strictures, tissue from the vaginal wall (vaginal flap urethroplasty) or buccal mucosa may be used to reconstruct and widen the urethral channel. This technique helps ensure a robust and flexible repair.
Procedure details:
- Dissection: Careful dissection is performed to expose the affected urethral segment.
- Resection or Incision: The scarred or strictured tissue is either removed or incised to open up the urethral lumen.
- Reconstruction: The defect is repaired using local tissue or a graft, ensuring that the new urethral lining is smooth and adequately wide to allow normal urine flow.
Postoperative care:
- Catheterization: A temporary urinary catheter is typically placed to ensure proper drainage and support the reconstructed urethra during healing.
- Follow-Up: Regular monitoring is essential to check for any recurrence of the stricture and to assess urinary function
Outcomes and Ccnsiderations
- Efficacy:
- When performed by an experienced surgeon, urethroplasty can offer a durable solution with significant improvement in urinary symptoms and quality of life.
- Risks and complications:
- As with any surgery, potential risks include infection, bleeding, and recurrence of the stricture.
- Adequate preoperative planning and meticulous surgical technique help minimize these risks.
Long-term management and follow-up
- Regular monitoring to check for recurrence.
- Pelvic floor therapy to strengthen muscles and improve urinary function.
- Lifestyle modifications, such as maintaining hydration and preventing infections.
Summary
Female urethral stricture is a narrowing of the urethra, often caused by scarring from infections, trauma, or previous surgeries. This condition can lead to symptoms like a weak urine stream, difficulty in fully emptying the bladder, and recurrent urinary tract infections. Diagnosis typically involves a physical examination, imaging studies, uroflowmetry, and cystoscopy. Treatment options range from conservative approaches, such as catheterization and urethral dilation, to surgical procedures like urethroplasty for more complex or recurrent cases.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply