High bladder neck or bladder neck elevation elevation (HBN, BNE) is a condition where the bladder neck, which is the area where the bladder connects to the urethra, is positioned higher than normal. This anatomical variation can lead to various urinary problems, including difficulty in urination, incomplete bladder emptying, and urinary retention. It is often identified through imaging studies like cystoscopy or urodynamic testing.
Effective treatment requires a thorough evaluation by a urologist to determine the underlying cause and appropriate intervention tailored to the patient’s specific condition.
FAQs and unswers
PNE, like BPH (benign prostate hyperplasia), causes urination difficulties. In severe cases, surgical treatment is required. I have tried to briefly summarize frequently asked questions and answers about this disease below.
What is high bladder neck?
Answer: Bladder neck elevation is a condition where the bladder neck, the area connecting the bladder to the urethra, is positioned higher than normal. This can lead to urinary issues such as difficulty urinating, incomplete bladder emptying, and urinary retention.
What causes of BNE?
Answer: It can be congenital (present from birth) or acquired due to factors such as surgeries, radiation therapy, pelvic trauma, or conditions like benign prostatic hyperplasia (BPH) in men.
What are the symptoms?
Answer: Symptoms include a weak urine stream, straining to urinate, frequent urination, and a sensation of incomplete bladder emptying. Severe cases can result in urinary tract infections and bladder stones due to residual urine.
How is HBN diagnosed?
Answer: Diagnosis is typically made through imaging studies such as cystoscopy, urodynamic testing, and sometimes MRI or CT scans to assess the anatomy of the bladder and urethra.
What are the treatment options?
Answer: Treatment options include:
Medications: Alpha-blockers (e.g., tamsulosin, alfuzosin) to relax bladder neck muscles.
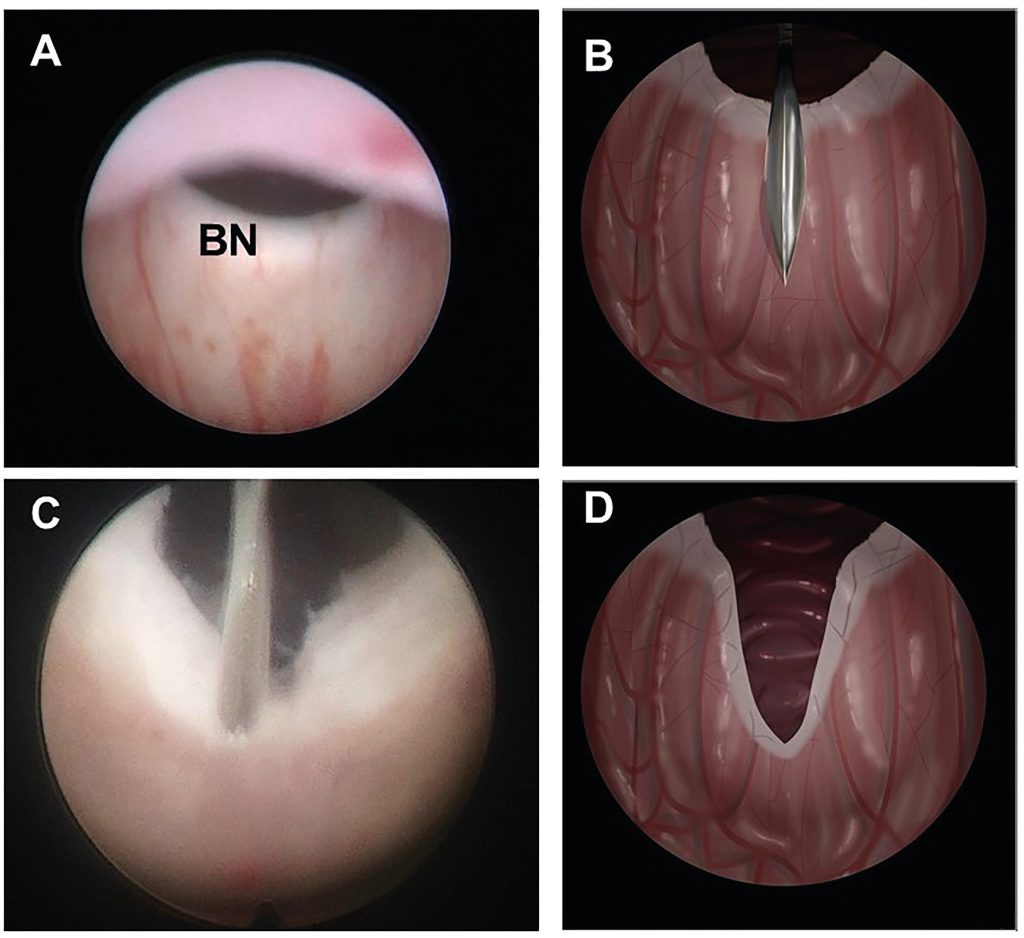
Minimally Invasive Procedures: Balloon dilation or transurethral resection of the bladder neck (TURBN).
Surgery: Bladder neck incision or suspension to correct the anatomical position. This operation is called as a trasurethral incision of the prostate (TUIP) at 05 and 07 o’clock levels. This procedure can be performed by holmium laser (HOLEP).
Lifestyle Modifications: Increased fluid intake, timed voiding schedules, and pelvic floor exercises.
Are medications effective for treating?
Answer: Yes, medications like alpha-blockers can be effective in relaxing the muscles of the bladder neck, making urination easier for some patients. However, the effectiveness varies depending on the severity and underlying cause.
What minimally invasive procedures are available?
Answer: Procedures such as balloon dilation, which widens the bladder neck, and transurethral resection of the bladder neck (TURBN), which removes obstructive tissue, are available to improve urinary flow.
When is surgery necessary for HBN?
Answer: Surgery is considered when other treatments, such as medications and minimally invasive procedures, are ineffective. Surgical options aim to correct the anatomical position and improve urinary flow.
Can lifestyle changes help manage?
Answer: Yes, lifestyle changes can help manage symptoms. These include increasing fluid intake, following a timed voiding schedule, and performing pelvic floor exercises to strengthen the muscles supporting the bladder.
What should I expect after treatment?
Answer: After treatment, most patients experience improved urinary flow and a reduction in symptoms. However, follow-up care is essential to monitor for any complications or recurrence of symptoms. Your healthcare provider will provide specific instructions based on the treatment received.
Can HBN recur after treatment?
Answer: While treatment is often effective, there is a possibility of recurrence, especially if the underlying cause is not fully addressed. Regular follow-up with your healthcare provider is important to monitor your condition and manage any recurring symptoms promptly.
Who should I consult if I suspect I have BNE?
Answer: If you suspect you have high bladder neck, you should consult a urologist, a specialist in urinary tract and male reproductive system disorders. They can provide a thorough evaluation and recommend appropriate treatment options.
FAQs about complications of treatment for BNE
Surgical treatment of PNE is a minimally invasive endoscopic procedure. There may be very rare and minimal complications. We have been performing these methods very successfully for many years with the HOLEP and TUR methods. We can list them as follows:
What are the potential complications of medications used to treat?
Answer: Medications such as alpha-blockers can cause side effects including dizziness, headaches, fatigue, nasal congestion, and retrograde ejaculation (where semen enters the bladder instead of exiting through the urethra).
What are the risks associated with minimally invasive procedures?
Answer: Risks of minimally invasive procedures like balloon dilation or transurethral resection (TURBN) include bleeding, infection, urinary incontinence, and urethral stricture (narrowing of the urethra).
What complications can arise from surgery?
Answer: Surgical complications may include:
- Bleeding: Excessive bleeding during or after surgery.
- Infection: Postoperative infections requiring antibiotics.
- Urinary Incontinence: Loss of bladder control.
- Scarring and Stricture: Formation of scar tissue leading to narrowing of the urethra.
- Sexual Dysfunction: Issues such as erectile dysfunction or retrograde ejaculation.
How common are complications from treatments?
Answer: The frequency of complications varies depending on the treatment type and individual patient factors. Minimally invasive procedures generally have a lower risk of complications compared to more invasive surgical interventions. Discussing risks with your healthcare provider can provide a clearer picture based on your specific situation.
Can lifestyle modifications to treat the disease have complications?
Answer: Lifestyle modifications are generally safe, but some individuals might experience discomfort or difficulty adhering to new routines, such as timed voiding schedules or performing pelvic floor exercises.
How can I reduce the risk of complications from treatment?
Answer: To minimize risks, follow your healthcare provider’s pre- and post-treatment instructions carefully, maintain good hygiene, stay hydrated, avoid strenuous activities until fully healed, and attend all follow-up appointments.
What should I do if I experience complications after treatment?
Answer: If you experience any complications such as severe pain, heavy bleeding, signs of infection (fever, chills, or foul-smelling urine), or difficulty urinating, contact your healthcare provider immediately for evaluation and management.
Can complications from treatment be managed effectively?
Answer: Yes, most complications can be managed effectively with prompt medical attention. Early detection and treatment of complications are crucial for the best outcomes.
Will complications affect the long-term success of my treatment?
Answer: While complications can impact the immediate recovery process, they do not necessarily affect the long-term success of the treatment if addressed promptly and properly. Regular follow-up and adherence to treatment plans are important.
Are there any long-term complications associated with the treatment?
Answer: Long-term complications can include persistent urinary symptoms, chronic urinary tract infections, and sexual dysfunction. Ongoing management and regular check-ups with your healthcare provider can help mitigate these issues.
What follow-up care is needed after treatment to monitor for complications?
Answer: Follow-up care typically includes regular visits to your healthcare provider to monitor healing, assess urinary function, and detect any early signs of complications. Imaging studies and urine tests may be conducted as needed.
How can I prepare for treatment to minimize complications?
Answer: Preparation may include:
- Discussing your medical history and any current medications with your doctor.
- Following any preoperative instructions such as fasting or bowel preparation.
- Arranging for post-treatment care and support at home.
- Ensuring you understand the procedure, potential risks, and post-treatment care instructions.
Summary
PNE is a rare disease. Very successful results are obtained with endoscopic surgery in severe symptomatic cases. Retrograde ejaculation may occur at a very low rate in young and single men after such surgical interventions.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE

Leave a Reply