Benign Prostatic Hyperplasia (BPH) is a common, non-cancerous enlargement of the prostate gland that affects many men as they age. Though not life-threatening, BPH can significantly impact quality of life due to its effects on urinary function. Understanding how BPH develops is crucial for early diagnosis and effective management. This overview explores the underlying mechanisms, risk factors, and progression of this prevalent condition.
Mechanisms of development of BPH
Here’s a clear breakdown of the mechanisms involved in the development of BPH:
1. Hormonal Changes with Age
- Dihydrotestosterone (DHT): As men age, testosterone levels slightly decline, but DHT levels often remain high in the prostate.
- DHT stimulates prostate cell growth, particularly in the transition zone, leading to gland enlargement.
- Estrogen may also play a role by increasing androgen receptor sensitivity in older men, enhancing DHT effects.
2. Cellular Proliferation and Apoptosis Imbalance
- BPH results from an imbalance between cell growth (proliferation) and cell death (apoptosis).
- Increased cell proliferation and reduced apoptosis lead to the accumulation of stromal (supportive) and epithelial (glandular) cells.
3. Inflammation and Cytokines
- Chronic inflammation in the prostate may contribute to BPH development.
- Inflammatory cells release cytokines and growth factors that promote tissue remodeling and further growth.
4. Stromal-Epithelial Interactions
- The interaction between stromal (connective tissue) and epithelial (glandular) cells regulates growth.
- Disruption in these interactions due to aging or inflammation can lead to abnormal tissue proliferation.
5. Growth Factors
- Several growth factors are involved, such as:
- Fibroblast Growth Factor (FGF)
- Insulin-like Growth Factor (IGF)
- Transforming Growth Factor-beta (TGF-β)
- These promote tissue regeneration and enlargement when unregulated.
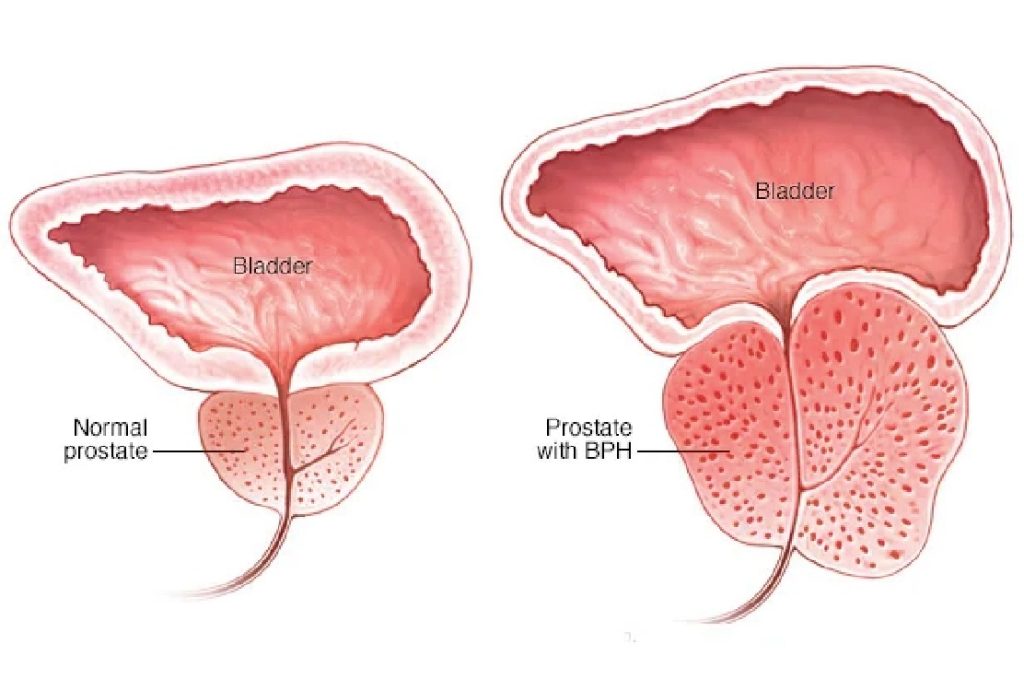
Location of Growth
- BPH primarily affects the transition zone of the prostate, which surrounds the urethra.
- Growth in this area leads to urethral compression, resulting in urinary symptoms.
Is age important for development of BPH?
Yes, age is one of the most important risk factors for the development of BPH.
As men get older, the likelihood of developing BPH increases significantly:
- By age 40, about 20% of men have some prostate enlargement.
- By age 60, this increases to around 50%.
- By age 80, up to 90% of men may be affected.
This age-related growth is thought to be linked to hormonal changes, particularly an increase in DHT, which promotes prostate cell growth.
Is it possible to prevent the development of BPH?
While BPH cannot be completely prevented, certain lifestyle choices and early interventions may reduce the risk or slow its progression. Here are some strategies that may help:
- Maintain a Healthy Weight: Obesity is associated with a higher risk of BPH. Regular physical activity and a balanced diet can help reduce this risk.
- Eat a Prostate-Friendly Diet: Diets rich in fruits, vegetables, and healthy fats (like those found in fish) may lower the risk. Limiting red meat and high-fat dairy products may also help.
- Limit Alcohol and Caffeine: These can irritate the bladder and worsen urinary symptoms, potentially speeding up symptom onset.
- Exercise Regularly: Physical activity improves hormone balance and reduces inflammation, both of which are protective factors.
- Manage Hormonal Health: Because BPH is linked to hormonal changes (especially dihydrotestosterone or DHT), keeping your hormones in balance through healthy lifestyle choices can be beneficial.
- Regular Check-Ups: Monitoring prostate health with your doctor can catch early signs and allow for early management, which may slow progression.
Although these steps can’t guarantee prevention, they contribute to overall prostate health and may delay or reduce the severity of BPH symptoms.
What do we do to reduce symptoms related to BPH?
To reduce symptoms related to BPH, you can use a combination of lifestyle changes, medications, and in some cases, procedures. Here’s a breakdown of effective strategies:
Lifestyle Changes
These are usually the first step and are often effective for mild symptoms:
- Limit fluid intake before bed to reduce nighttime urination.
- Avoid caffeine and alcohol, which can irritate the bladder.
- Practice double voiding (urinate, wait a few minutes, then try again) to empty the bladder more fully.
- Stay active — regular exercise helps improve urinary function.
- Avoid decongestants or antihistamines, which can tighten the muscles around the urethra.
Medications
If lifestyle changes aren’t enough, doctors may prescribe:
- Alpha blockers (e.g., tamsulosin, alfuzosin): Relax prostate and bladder neck muscles to improve urine flow.
- 5-alpha-reductase inhibitors (e.g., finasteride, dutasteride): Shrink the prostate by lowering DHT hormone levels.
- Combination therapy: Using both types for better symptom control.
- Phosphodiesterase-5 inhibitors (e.g., tadalafil): Can help with both BPH and erectile dysfunction.
Minimally Invasive Procedures or Surgery
For moderate to severe symptoms or when medications fail:
- TURP (Transurethral Resection of the Prostate): The most common surgery to remove part of the prostate.
- Laser therapy: Destroys or removes prostate tissue.
- UroLift system: Implants that lift and hold the enlarged prostate tissue out of the way.
- Prostatic artery embolization (PAE): Blocks blood flow to reduce prostate size.
Mental and Emotional Support
BPH symptoms can impact sleep, mood, and quality of life. Don’t hesitate to:
- Join a support group
- Discuss treatment goals with your doctor
- Address related stress or anxiety
Summary
Benign Prostatic Hyperplasia develops as a result of non-cancerous enlargement of the prostate gland, most commonly due to age-related hormonal changes, especially increased levels of dihydrotestosterone (DHT). As men age, prostate cells multiply, gradually enlarging the gland and pressing against the urethra, leading to urinary symptoms such as difficulty starting urination, weak stream, and frequent urination. The exact cause is not fully understood, but age, hormonal balance, and genetics play key roles.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul – TURKIYE


Leave a Reply