Partial cystectomy (PC) is a surgical procedure used to treat bladder cancer by removing only the part of the bladder affected by the tumor, rather than the entire bladder. This approach is typically considered when the cancer is localized to a specific area of the bladder and hasn’t spread to other parts.
The goal of partial cystectomy is to eliminate the cancer while preserving as much bladder function as possible. It is often followed by additional treatments, such as chemotherapy or radiation, to reduce the risk of recurrence.
What is “partial cystectomy”?
Partial cystectomy for bladder cancer is a surgical procedure in which only a portion of the bladder is removed, specifically the area containing the cancerous tumor. This type of surgery is typically considered when the cancer is localized and hasn’t spread extensively within the bladder or to other parts of the body. By removing just the affected part, the surgeon aims to preserve as much of the bladder’s function as possible, allowing the patient to maintain normal urinary function. After the surgery, additional treatments such as chemotherapy or radiation may be recommended to prevent the recurrence of cancer.
Only a small percentage of bladder cancer cases are suitable for PC, generally estimated to be around 5-10% of all bladder cancer patients.
Indications of PC
Partial cystectomy for bladder cancer is indicated under specific conditions, including:
- Localized Tumors: The cancer is confined to a specific, limited area of the bladder and hasn’t spread to multiple sites within the bladder or beyond.
- Muscle-Invasive Cancer: The cancer has invaded the muscle layer of the bladder but is still limited to a small, resectable area.
- Favorable Tumor Location: The tumor is situated in an area of the bladder that allows for safe and complete removal without significantly compromising bladder function. Tumors located away from the bladder neck or ureters are more suitable for partial cystectomy.
- Absence of Multifocal Disease: The patient does not have multiple tumors or widespread carcinoma in situ (a flat, high-grade tumor confined to the bladder lining).
- Patient’s Overall Health: The patient is in good general health, making them a suitable candidate for surgery, and desires to preserve as much bladder function as possible.
- Desire for Bladder Preservation: The patient prefers to avoid radical cystectomy (complete removal of the bladder) to maintain urinary function and quality of life.
- Potential for Complete Resection: There is a high likelihood that the entire tumor can be removed with clear margins, reducing the risk of recurrence.
Contrainndications of PC
Partial cystectomy for bladder cancer has several contraindications, meaning it may not be a suitable option in certain cases. These contraindications include:
- Multifocal Disease: If the bladder cancer is present in multiple areas of the bladder, partial cystectomy is not appropriate, as removing only part of the bladder would leave other cancerous areas untreated.
- Carcinoma In Situ (CIS): Widespread or multifocal carcinoma in situ, a high-grade flat tumor that affects the bladder lining, is a contraindication, as it increases the risk of recurrence in the remaining bladder tissue.
- Poor Tumor Location: Tumors located near critical areas like the bladder neck, ureteral orifices, or the trigone (a triangular area at the base of the bladder) make partial cystectomy challenging without compromising bladder function or complete removal of the cancer.
- Advanced or Large Tumors: If the tumor is large, deeply invasive, or has spread beyond the bladder (e.g., to lymph nodes or distant organs), partial cystectomy is not appropriate. Radical cystectomy, which involves removing the entire bladder, is typically recommended in these cases.
- High Risk of Recurrence: Patients with a high risk of cancer recurrence or those who have had recurrent tumors may not be suitable candidates for partial cystectomy, as the procedure may not adequately reduce the risk of the cancer returning.
- Poor General Health: Patients with significant comorbidities or those who are not fit for major surgery may not be good candidates for partial cystectomy, as the benefits of the procedure may not outweigh the risks.
- Inability to Achieve Clear Margins: If there is a high likelihood that the tumor cannot be completely removed with clear margins (i.e., no cancer cells left at the edges of the removed tissue), partial cystectomy may not be advisable, as it increases the risk of recurrence.
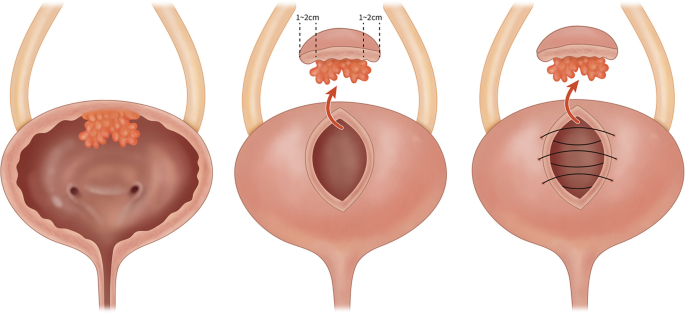
How to do PC?
Partial cystectomy can be performed using open, laparoscopic, or robotic techniques Here’s a general overview of how the procedure is performed:
Preoperative Preparation:
- Imaging and Evaluation: Before surgery, imaging studies such as CT scans, MRI, or cystoscopy are conducted to assess the tumor’s size, location, and extent.
- Anesthesia: The patient is placed under general anesthesia, ensuring they are unconscious and pain-free during the surgery.
- Bladder Preparation: A catheter is usually inserted into the bladder to drain urine during the procedure.
Surgical Procedure:
- Incision: An incision is made in the lower abdomen to access the bladder. The incision can be made either as a traditional open surgery or through minimally invasive techniques like laparoscopic or robotic-assisted surgery.
- Bladder Exposure: The bladder is carefully exposed, and the area containing the tumor is identified. The surgeon assesses the tumor’s location to determine the extent of bladder removal needed.
- Tumor Resection: The surgeon removes the portion of the bladder containing the tumor along with a margin of healthy tissue to ensure that all cancerous cells are removed. This step is crucial to minimize the risk of recurrence.
- Bladder Reconstruction: After removing the tumor, the remaining bladder tissue is sutured back together. The surgeon ensures that the bladder retains its function and that there are no leaks from the surgical site.
- Lymph Node Evaluation (if needed): In some cases, nearby lymph nodes may be removed and examined to check for the spread of cancer. This step helps determine the extent of the disease and the need for additional treatments.
Postoperative Care:
- Recovery and Monitoring: The patient is monitored closely in the hospital for a few days to manage pain, monitor for complications, and ensure proper healing.
- Catheter Management: The bladder may be drained with a catheter for several days to allow it to heal.
- Follow-up and Additional Treatment: After surgery, follow-up appointments are scheduled to monitor recovery and bladder function. Additional treatments, such as chemotherapy or radiation, may be recommended to reduce the risk of cancer recurrence.
Recovery:
- Hospital Stay: The patient typically stays in the hospital for several days to a week, depending on the extent of the surgery and the patient’s overall health.
- Return to Normal Activities: Full recovery may take several weeks, during which the patient should avoid heavy lifting and strenuous activities.
Partial cystectomy is a complex procedure that requires careful patient selection and skilled surgical expertise. The goal is to remove the cancer while preserving as much bladder function as possible.
Complications of partial cystectomy
Partial cystectomy for bladder cancer, like any major surgery, carries a risk of complications. Some of the potential complications include:
1. Bleeding:
- Intraoperative Bleeding
- Postoperative Bleeding
2. Infection:
- Wound Infection
- Urinary Tract Infection (UTI)
3. Bladder Issues:
- Urinary Incontinence
- Urinary Retention
- Decreased Bladder Capacity
4. Bladder Leakage:
- Urine Leak from Surgical Site: Urine may leak from the resected area, requiring additional intervention to repair the leak.
5. Fistula Formation:
- Vesicovaginal Fistula
- Vesicoenteric Fistula
6. Bowel Obstruction:
- Postoperative Ileus: Temporary paralysis of the bowel, leading to delayed return of bowel function and possible obstruction.
7. Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE):
- Formation of blood clots in the legs (DVT) that can travel to the lungs (PE), posing serious health risks.
8. Anastomotic Stricture:
- Narrowing at the site where the bladder is reconstructed, leading to difficulty urinating and potential need for further procedures.
9. Cancer Recurrence:
- Local Recurrence
- Metastasis
10. General Surgical Risks:
- Anesthesia Complications
- Cardiovascular Complications
11. Chronic Pain:
- Persistent pain at the surgical site, which may require pain management strategies.
12. Reduced Sexual Function:
- Erectile Dysfunction
- Sexual Dysfunction in Women
While these complications are possible, many patients recover well from partial cystectomy with proper care and monitoring. The risks are weighed against the benefits of preserving the bladder and maintaining quality of life.
Neoadjuvant, adjuvat or radiotherapy in conjunction with PC
The use of neoadjuvant therapy, adjuvant therapy, or radiotherapy in conjunction with partial cystectomy for bladder cancer depends on the specific characteristics of the cancer and the patient’s overall health. Here’s a brief overview of how these therapies might be used:
1. Neoadjuvant Therapy:
- Purpose: Administered before surgery to shrink the tumor, making it easier to remove and reducing the likelihood of cancer spread.
- Chemotherapy: Commonly used in muscle-invasive bladder cancer to improve surgical outcomes and reduce the risk of recurrence.
- Indications: Considered for patients with muscle-invasive or high-grade tumors that are still confined to the bladder.
2. Adjuvant Therapy:
- Purpose: Given after surgery to eliminate any remaining cancer cells, thereby reducing the risk of recurrence.
- Chemotherapy: May be recommended if there are concerns about residual cancer or if the cancer has features that suggest a high risk of recurrence.
- Radiotherapy: Less commonly used after partial cystectomy, but may be considered in cases where surgical margins are close or if there’s a high risk of local recurrence.
3. Radiotherapy:
- Standalone or Combined: Radiotherapy can be used either as a primary treatment for bladder cancer or as an adjunct to surgery.
- Postoperative Radiotherapy: May be used in select cases where there’s concern about residual cancer or in cases of close or positive surgical margins.
- Considerations: The decision to use radiotherapy must take into account the potential impact on bladder function and the patient’s overall health.
The decision to use these therapies is based on individual patient factors, including tumor stage, grade, and overall health, and should be discussed with a multidisciplinary medical team.
Prognosis of PC
The prognosis of partial cystectomy for bladder cancer depends on several factors, including the stage and grade of the cancer, the success of the surgery, and the use of additional treatments. Here’s a summary of key factors influencing the prognosis:
1. Tumor Stage and Grade:
- Early-Stage, Low-Grade Tumors: Patients with early-stage (T1 or T2) and low-grade tumors generally have a better prognosis, as the cancer is less likely to spread or recur.
- Muscle-Invasive, High-Grade Tumors: The prognosis is more guarded for muscle-invasive or high-grade tumors, as these are more aggressive and have a higher risk of recurrence or metastasis.
2. Surgical Margins:
- Clear Margins: If the tumor is completely removed with clear surgical margins (no cancer cells at the edge of the removed tissue), the prognosis is more favorable, with a lower risk of recurrence.
- Positive or Close Margins: If cancer cells are found at the margins or if the margins are close, there is a higher risk of recurrence, potentially worsening the prognosis.
3. Cancer Recurrence:
- Local Recurrence: Bladder cancer has a tendency to recur, even after partial cystectomy. Recurrence can occur in the remaining bladder tissue, which may require further treatment.
- Distant Metastasis: If the cancer spreads to other parts of the body (metastasis), the prognosis becomes poorer.
4. Use of Adjuvant Therapies:
- Chemotherapy and Radiotherapy: The use of adjuvant chemotherapy or radiotherapy can improve prognosis by reducing the risk of recurrence, especially in high-risk cases.
5. Overall Health and Bladder Function:
- Bladder Function: Preserving bladder function is a significant advantage of partial cystectomy, contributing to a better quality of life.
- Patient’s Health: The patient’s overall health and ability to recover from surgery also impact the prognosis.
6. Surveillance:
- Regular Monitoring: Ongoing surveillance with cystoscopy and imaging is crucial to detect any recurrence early, which can improve long-term outcomes.
General Prognosis:
- Favorable Prognosis: For patients with early-stage, localized bladder cancer that is fully resected with clear margins, the long-term survival rates are generally favorable.
- Moderate to Guarded Prognosis: Patients with higher-stage or higher-grade tumors, those with close or positive margins, or those who experience recurrence may have a more guarded prognosis, depending on the success of additional treatments.
Summary
Partial cystectomy for bladder cancer is a surgical procedure in which only the portion of the bladder containing the cancerous tumor is removed, rather than the entire bladder. This approach is typically used when the cancer is localized and hasn’t spread to other parts of the bladder or body. The goal is to eliminate the tumor while preserving as much bladder function as possible. While it offers the advantage of maintaining urinary function, the procedure carries risks such as bleeding, infection, reduced bladder capacity, and potential recurrence of cancer. It is suitable only for select patients who meet specific criteria.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply