Penile cancer is a rare type of cancer that forms in the tissues of the penis, most commonly in the cells of the skin. It primarily affects men over the age of 50 but can occur at any age. The most common form is squamous cell carcinoma, which develops in the flat cells lining the penis. Risk factors include HPV infection, smoking, poor hygiene, and conditions like phimosis. Early detection is crucial, as the cancer can be treated effectively with surgery, radiation, or chemotherapy if caught in its early stages.
What is penile cancer?
Penile cancer is a rare form of cancer that develops in or on the penis, typically originating in the skin or tissues of the organ. The most common type is squamous cell carcinoma, which arises in the flat cells of the skin covering the penis. It can also occur in other cell types, but these cases are less frequent.
The cancer generally starts as a growth, sore, or lump, often near the tip or foreskin, but it can appear anywhere on the penis. If left untreated, it can spread to other parts of the body, such as the lymph nodes or organs.
Risk factors for penile cancer
Several risk factors can increase the likelihood of developing it. Here are the main risk factors:
- HPV infection
- Uncircumcised penis
- Smoking
- Chronic ınflammation or infection
- Age
- Weakened immune system
- Poor hygiene
- Psoriasis treatments: Some medications used to treat psoriasis, especially those that suppress the immune system, have been linked to an increased risk of penile cancer.
- History of penile lesions or precancerous conditions
- Family history
Causes of penile cancer
The exact cause of penis cancer is not entirely known, but certain factors increase the likelihood of developing it. Here are some of the key causes and risk factors:
HPV infection: Particularly HPV-16 and HPV-18, are strongly associated with squamous cell carcinoma of the penis.
Smoking: Smoking can damage the DNA of cells. It also weakens the immune system.
Poor hygiene: Men who do not regularly clean under the foreskin (in uncircumcised men) may develop smegma, a substance that can cause chronic irritation and inflammation.
Phimosis: Phimosis is a condition where the foreskin is too tight to be retracted over the head of the penis. This can trap bacteria and cause infections, leading to chronic inflammation, which is a known risk factor for cancer.
Circumcision status: Penile cancer is more common in uncircumcised men. Studies suggest that men circumcised at birth or as young children have a significantly lower risk of developing penile cancer compared to those who are uncircumcised. This is thought to be related to the reduced risk of HPV infection and better hygiene.
Age: Penile cancer most often affects men over the age of 50, though it can occur in younger men.
Weakened ımmune system: Men with with HIV/AIDS or taking immunosuppressive medications are at higher risk of developing penile cancer.
Chronic ınflammation or infection: Conditions that cause long-term inflammation, such as balanitis (inflammation of the head of the penis) or chronic infections.
UV radiation treatment: Rarely, men who have had psoriasis treatment using ultraviolet (UV) light and a drug called psoralen may be at higher risk for developing penile cancer.
Sypmtoms of penis cancer
The symptoms of penile cancer can vary depending on the stage and type of cancer, but some common signs to watch for include:
- Lump or growth on the penis
- Sores or ulcers
- Changes in skin color or texture
- Bleeding
- Abnormal discharge
- Pain or tenderness
- Swelling or lumps in the groin
- Foul-smelling smegma
- Changes in the foreskin
- Unexplained weight loss or fatigue (advanced stages)
Diagnosis
The diagnosis of penile cancer typically involves a combination of physical examination, imaging tests, and biopsies.
Physical examination and history: Urologist will first perform a thorough physical examination of the penis, paying close attention to any unusual growths, sores, lumps, or skin changes. The groin and lymph nodes may also be checked for any signs of swelling or abnormalities, as cancer can spread to these areas. The doctor will ask about any symptoms, medical history and any known risk factors.
Biopsy: A biopsy is the definitive test to diagnose penile cancer.
Imaging tests
- Ultrasound: This can be used to check for enlarged lymph nodes in the groin area and to assess the depth of the tumor’s invasion into surrounding tissues.
- CT Scan (Computed Tomography): A CT scan of the abdomen and pelvis may be done to check if cancer has spread to nearby structures or lymph nodes.
- MRI (Magnetic Resonance Imaging): MRI can offer more detailed imaging to assess the extent of the tumor, particularly in the soft tissues.
- PET Scan (Positron Emission Tomography): Sometimes used to look for signs of cancer spread (metastasis) in the body.
Lymph node evaluation: Since penile cancer can spread to the lymph nodes, particularly in the groin, evaluating these nodes is crucial:
Blood tests: While blood tests are not typically used to diagnose penile cancer, they may be done to assess general health and check for markers of cancer spread or infection.
HPV testing: In some cases, testing for HPV (especially high-risk strains like HPV-16 and HPV-18) may be recommended to identify an underlying cause of the cancer.
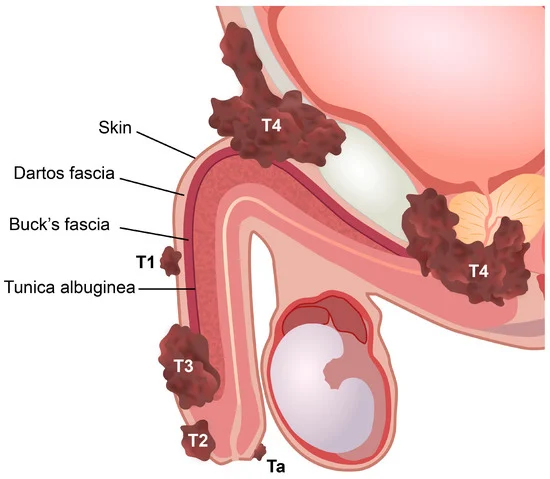
Staging of penile cancer
Once cancer is diagnosed, staging is performed to determine the extent of the disease. This includes:
Stage 0: Non-invasive cancer, localized to the surface of the skin.
Stage I: Cancer has invaded deeper tissues but remains within the penis.
Stage II: Cancer has spread to nearby tissues and possibly lymph nodes.
Stage III: Cancer has spread to lymph nodes or distant tissues.
Stage IV: Advanced cancer with widespread metastasis to distant organs.
Prevention
Here’s how you can lower the chances of developing this type of cancer:
- Get vaccinated against HPV.
- Consider circumcision (if medically advisable).
- Practice good personal hygiene, particularly if uncircumcised.
- Use condoms and practice safe sex.
- Quit smoking to reduce cancer risk.
- Attend regular medical check-ups and monitor for any changes.
- Manage chronic conditions like phimosis and diabetes.
Treatment of penile cancer
Treatment options for penile cancer typically include surgery, radiation therapy, chemotherapy, and sometimes a combination of these.
Surgery: Surgery is the most common and often the most effective treatment for penile cancer, particularly in its early stages. The type of surgery performed depends on the size, location, and extent of the cancer.
Radiation therapy: Radiation therapy uses high-energy rays (such as X-rays) to kill cancer cells or shrink tumors. It may be used in combination with surgery or as an alternative to surgery in certain cases.
Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop them from growing. For penile cancer, chemotherapy is typically used in more advanced cases or when cancer has spread to lymph nodes or distant organs.
Others: Immunotherapy, laser therapy, cryotherapy, reconstructive surgery.
Follow-up care
After treatment, regular follow-up visits are essential to monitor for any signs of recurrence. This often includes physical exams, imaging tests, and sometimes biopsies. Early detection of recurrence can help manage the cancer effectively.
Summary
Penile cancer is a rare form of cancer that develops in or on the penis, most commonly in the skin cells. It is most often caused by HPV infection, smoking, poor hygiene, and conditions like phimosis. Symptoms may include a growth, sore, or abnormal discharge on the penis, and the cancer can spread to nearby lymph nodes if left untreated. Treatment typically involves surgery, radiation therapy, chemotherapy, or immunotherapy, depending on the cancer’s stage. Prevention includes HPV vaccination, good hygiene, circumcision, and avoiding smoking. Early detection and treatment are crucial for better outcomes.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply