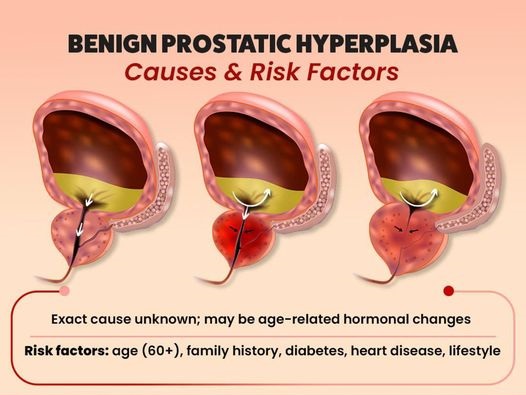
Benign Prostatic Hyperplasia (BPH) and diabetes mellitus are two prevalent conditions that often coexist, particularly in the aging male population. BPH, characterized by the non-cancerous enlargement of the prostate gland, can lead to urinary symptoms such as difficulty in urination, increased frequency, and nocturia. Diabetes mellitus, a metabolic disorder marked by chronic high blood sugar levels, can exacerbate these urinary symptoms due to its impact on nerve function and bladder control.
Emerging research suggests a potential bidirectional relationship where diabetes may increase the risk of BPH, and vice versa, through mechanisms involving hormonal imbalances, insulin resistance, and chronic inflammation. Understanding this interplay is crucial for effective management and treatment of both conditions, improving the quality of life for affected individuals.
Is there link between BPH and diabetes mellitus?
Yes, there is a significant link between BPH and diabetes mellitus. Several studies have identified a correlation between these two conditions, suggesting that diabetes can increase the risk of developing BPH and exacerbate its symptoms. Here are some key points that highlight this relationship:
- Insulin Resistance and Hyperinsulinemia: Diabetes mellitus, particularly type 2 diabetes, is associated with insulin resistance and elevated insulin levels (hyperinsulinemia). Insulin can promote cell growth and proliferation, potentially contributing to the enlargement of the prostate gland seen in BPH.
- Inflammation: Chronic inflammation, common in both diabetes and BPH, may play a role in linking the two conditions. High blood sugar levels in diabetes can lead to inflammatory responses that may also affect the prostate tissue, worsening BPH symptoms.
- Hormonal Changes: Diabetes can alter hormone levels, including those of testosterone and estrogen, which can influence prostate growth. An imbalance in these hormones is thought to contribute to the development and progression of BPH.
- Autonomic Nervous System Dysfunction: Diabetes can cause autonomic neuropathy, which affects the nerves that control the bladder and prostate. This can lead to worsening urinary symptoms and complications related to BPH.
- Metabolic Syndrome: Diabetes is often part of a broader metabolic syndrome that includes obesity, hypertension, and dyslipidemia. These factors are also associated with an increased risk of BPH, suggesting that metabolic health overall influences prostate health.
Understanding these connections can aid in the management and treatment of both BPH and diabetes, improving patient outcomes.
Severity of BPH symptoms in patients with diabetes mellitus
Patients with diabetes mellitus often experience more severe symptoms of BPH compared to those without diabetes. This increased severity can be attributed to several factors:
- Worsened Urinary Symptoms: Diabetes can cause bladder dysfunction due to autonomic neuropathy, leading to symptoms such as urinary frequency, urgency, nocturia, and incomplete bladder emptying. These symptoms overlap with and can intensify the symptoms of BPH.
- Increased Inflammation: Chronic high blood sugar levels in diabetes lead to increased inflammation, which can exacerbate the inflammation in the prostate associated with BPH, worsening its symptoms.
- Poor Glycemic Control: Patients with poorly controlled diabetes tend to have more severe BPH symptoms. Hyperglycemia can worsen bladder function and increase the severity of lower urinary tract symptoms (LUTS) commonly associated with BPH.
- Obesity and Metabolic Syndrome: Diabetic patients often have coexisting obesity and other elements of metabolic syndrome, which are risk factors for more severe BPH symptoms. Adipose tissue produces inflammatory cytokines and other factors that can promote prostate growth and inflammation.
- Insulin Resistance: Insulin resistance, commonly seen in type 2 diabetes, is associated with increased levels of insulin and growth factors that can contribute to prostate tissue growth and the worsening of BPH symptoms.
- Compromised Bladder Function: Diabetes can lead to detrusor muscle dysfunction (the muscle that contracts to empty the bladder), which may cause urinary retention and overflow incontinence. This can worsen the bladder outlet obstruction caused by BPH.
- Hormonal Imbalances: Diabetes can affect the levels of hormones such as testosterone and estrogen, which play a role in prostate growth and function. Imbalances in these hormones can exacerbate BPH symptoms.
Treatment of BPH in patients with diabetes mellitus
Treating BPH in patients with diabetes mellitus requires a comprehensive approach that addresses both conditions simultaneously to optimize patient outcomes. Here are some key strategies and considerations for treatment:
Lifestyle Modifications
- Diet and Exercise: Adopting a healthy diet and engaging in regular physical activity can help manage both diabetes and BPH. Weight loss and improved metabolic control can reduce the severity of BPH symptoms.
- Fluid Management: Managing fluid intake, especially before bedtime, can help reduce nocturia and other urinary symptoms.
Medical Management
- Alpha-Blockers: Medications such as tamsulosin and alfuzosin can relax the muscles of the prostate and bladder neck, improving urine flow and reducing symptoms. These drugs are generally safe for diabetic patients.
- 5-Alpha-Reductase Inhibitors: Drugs like finasteride and dutasteride can reduce the size of the prostate by blocking the conversion of testosterone to dihydrotestosterone (DHT). These medications can be effective but may take several months to show benefits.
- Combination Therapy: Using both alpha-blockers and 5-alpha-reductase inhibitors together can provide greater symptom relief than either drug alone.
- Anticholinergics: These medications can help manage overactive bladder symptoms, which are common in diabetic patients with BPH. Caution is needed as they can sometimes worsen urinary retention.
- Phosphodiesterase-5 Inhibitors: Tadalafil, used for erectile dysfunction, can also help reduce BPH symptoms and is beneficial for patients with concurrent diabetes and BPH.
Blood Sugar Control
- Optimized Diabetes Management: Maintaining good glycemic control is crucial. Poorly controlled diabetes can exacerbate BPH symptoms, so working closely with a healthcare provider to manage blood sugar levels is important.
Minimally Invasive Procedures
- Transurethral Microwave Thermotherapy (TUMT): This procedure uses microwave energy to reduce prostate tissue and can be an option for patients who do not respond well to medications.
- Transurethral Needle Ablation (TUNA): Radiofrequency energy is used to heat and destroy prostate tissue, providing symptom relief.
Surgical Options
- Transurethral Resection of the Prostate (TURP): This is a common surgical procedure for BPH that involves removing part of the prostate through the urethra. It is effective but may have a longer recovery time and potential complications, especially in diabetic patients.
- Laser Surgery: Procedures such as Holmium Laser Enucleation of the Prostate (HoLEP) or Photoselective Vaporization of the Prostate (PVP) use lasers to remove or vaporize prostate tissue. These options may have fewer complications and quicker recovery times.
Monitoring and Follow-Up
- Regular Check-Ups: Regular monitoring of both BPH symptoms and diabetes management is essential. Adjustments to treatment plans should be made based on symptom progression and changes in overall health.
- Patient Education: Educating patients about the importance of managing both conditions and recognizing symptom changes can improve adherence to treatment and outcomes.
Indication of surgery for BPH in diabetic patients
BPH patients with diabetes mellitus may have a higher likelihood of requiring surgical treatment compared to non-diabetic BPH patients. This increased need can be attributed to several factors:
- Severity of Symptoms: Diabetes can worsen urinary symptoms due to autonomic neuropathy, poor bladder function, and increased inflammation, leading to more severe BPH symptoms that may not respond adequately to medication alone.
- Reduced Efficacy of Medications: In some cases, diabetic patients may not respond as well to standard BPH medications due to underlying metabolic and hormonal issues. This can make surgical intervention a more viable option.
- Bladder Dysfunction: Diabetes can cause bladder dysfunction, including decreased bladder contractility and overactive bladder, which can complicate BPH management and necessitate surgical treatment to relieve obstruction.
- Complications from Poor Glycemic Control: Poorly controlled diabetes can exacerbate BPH symptoms and lead to complications such as recurrent urinary tract infections or bladder stones, which might require surgical intervention.
- Faster Disease Progression: The interplay between diabetes and BPH can lead to a more rapid progression of BPH, potentially increasing the need for surgery.
Summary
BPH and diabetes mellitus are often interlinked, particularly in older men. Research indicates that diabetes can increase the risk and severity of BPH through mechanisms such as insulin resistance, chronic inflammation, hormonal imbalances, and autonomic neuropathy. Diabetic patients are more likely to experience worsened urinary symptoms, including frequency, urgency, and nocturia, due to these shared pathways. Effective management of both conditions involves a combination of lifestyle changes, medical therapies, and careful monitoring to mitigate symptoms and improve patient outcomes.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply