Skene gland cyst surgery is a minor surgical procedure performed to treat cysts that develop in the Skene’s glands—also known as the paraurethral glands. These small glands, located on either side of the urethral opening, play a role in female lubrication. When their ducts become blocked, fluid can accumulate, leading to the formation of a cyst. While many Skene gland cysts are asymptomatic and resolve on their own, larger or symptomatic cysts may require surgical intervention to relieve discomfort, prevent infection, or rule out other conditions.
This procedure typically involves drainage, marsupialization, or complete excision of the cyst, depending on its size, recurrence, and the patient’s overall health. The surgery is generally safe, minimally invasive, and performed under local or general anesthesia, with most patients recovering quickly.
What is the skene (paraurethral) gland?
The Skene glands, also known as the paraurethral glands, are small glands located on either side of the urethral opening in people assigned female at birth. These glands are part of the female urogenital system and are considered the female equivalent of the male prostate.
They have small ducts that open into the urethra and are thought to play a role in producing fluid that helps lubricate the urethral area. In some individuals, they may also contribute to what’s sometimes referred to as “female ejaculation” during sexual activity, although this is still being studied.
If the ducts of the Skene glands become blocked, fluid can build up, forming a Skene gland cyst. These cysts are usually benign but can sometimes become painful, infected, or large enough to interfere with urination or sexual activity, which may require medical or surgical treatment.
Causes of skene gland cyst
A Skene gland cyst forms when the ducts of the Skene glands—located near the urethral opening—become blocked or obstructed, leading to a buildup of fluid. This blockage can occur due to several reasons:
- Infection or Inflammation: Bacterial infections (e.g., urinary tract infections or sexually transmitted infections) can inflame the area, causing swelling or scarring that blocks the gland’s duct.
- Trauma or Injury: Physical trauma from childbirth, catheterization, or sexual activity can damage or irritate the glands, potentially leading to duct obstruction.
- Hormonal Changes: Shifts in hormone levels, especially during puberty or menopause, can affect glandular secretions and possibly lead to cyst formation.
- Chronic Irritation: Ongoing irritation from hygiene products, tight clothing, or poor genital hygiene might contribute to gland blockage.
- Congenital Abnormalities: Rarely, some people may be born with structural abnormalities in the gland or its ducts that make cyst formation more likely.
Symptoms of skene gland cysts
Many Skene gland cysts are small and painless, causing no symptoms. However, when symptoms do occur, they may include:
- Swelling near the urethral opening: A visible or palpable lump on either side of the urethra.
- Pain or discomfort: Especially during urination, sexual activity, or when sitting.
- Difficulty urinating: A feeling of incomplete emptying, slow urine stream, or urinary retention if the cyst presses against the urethra.
- Frequent urinary tract infections (UTIs): Caused by partial blockage or irritation of the urethra.
- Tenderness or pressure: Localized to the lower genital area, especially if the cyst is inflamed.
- Discharge from the urethra: May occur if the cyst becomes infected and drains spontaneously.
- Fever or redness (in infected cysts): Signs of an abscess or infection, which require medical attention.
Diagnosis of skene gland cysts
Diagnosis is usually based on clinical evaluation, but sometimes additional tests may be needed to confirm the diagnosis or rule out other conditions.
1. Medical History
- Your healthcare provider will ask about:
- Symptoms (pain, swelling, urination issues, discharge)
- Duration of symptoms
- History of infections, trauma, or surgeries
- Sexual and urinary health
2. Physical Examination
- A pelvic exam is performed to:
- Inspect the area around the urethral opening
- Feel for any lumps or swelling near the Skene glands
- Assess tenderness, discharge, or signs of infection
3. Urinalysis or Urine Culture
- To check for:
- Urinary tract infections (UTIs)
- Presence of bacteria or white blood cells in the urine
4. Imaging (if needed)
- Usually done if the cyst is large, recurrent, or unclear:
- Ultrasound – to visualize the cyst and its contents
- MRI or CT scan – rarely needed, but may be used for complex or deep cysts
5. Cyst Fluid Analysis or Biopsy (in certain cases)
- If there’s any concern about infection or rare tumors:
- A sample of fluid may be taken for lab testing
- A biopsy might be done to rule out malignancy (extremely rare)
Differential diagnosis
Urologist may also want to rule out other conditions with similar symptoms, such as:
- Urethral diverticulum
- Bartholin gland cyst
- Abscess
- Vaginal or urethral tumors
Indications for surgical treatment
Surgery is usually not the first line of treatment for small, asymptomatic Skene gland cysts. However, surgical intervention is indicated when:
1. Symptomatic Cyst
- Causing pain, discomfort, or pressure in the vaginal or urethral area
- Interfering with daily activities, urination, or sexual function
2. Urinary Obstruction
- When the cyst is large enough to compress the urethra, leading to:
- Difficulty urinating
- Slow or weak urinary stream
- Urinary retention
3. Recurrent Infections
- Repeated urinary tract infections (UTIs) associated with the cyst
- Cyst becomes recurrently inflamed or infected
4. Abscess Formation
- The cyst becomes infected, leading to:
- Painful swelling
- Redness, warmth, and possibly fever
- Formation of pus or spontaneous drainage
5. Failure of Conservative Treatment
- When non-surgical methods such as:
- Warm compresses
- Antibiotics
- Aspiration
do not resolve the cyst or symptoms
6. Uncertainty in Diagnosis
- If there is concern about malignancy or the diagnosis is unclear, surgical removal may be done for biopsy and histological examination.
Surgical treatment of skene gland cysts
Surgical management is considered when the cyst is large, symptomatic, infected, or recurrent. The goals are to relieve symptoms, prevent complications, and, in some cases, confirm the diagnosis through tissue analysis.
Types of Surgery
1. Incision and Drainage
- A small cut is made to drain fluid or pus from the cyst.
- Often used for infected cysts or abscesses.
- Quick relief, but high chance of recurrence since the cyst lining remains.
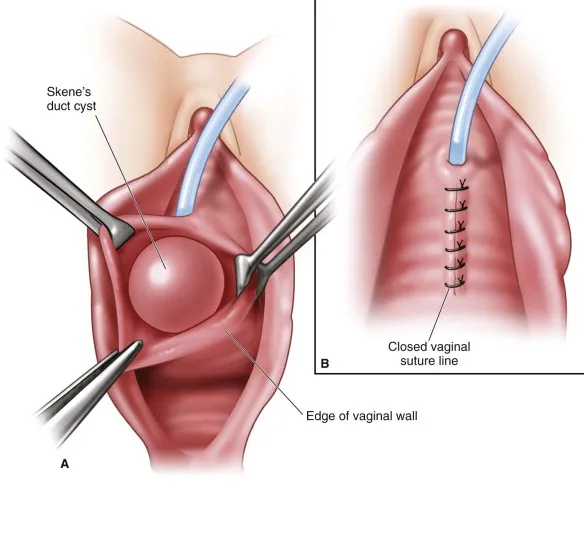
2. Marsupialization
- The cyst is opened, and the edges of the cyst wall are sutured to the skin to keep the opening permanently open.
- This allows continuous drainage and helps prevent recurrence.
- Often used for recurrent or large cysts.
3. Excision (Complete Removal)
- The entire Skene gland and cyst are surgically removed.
- Usually done if:
- The cyst keeps coming back
- There’s suspicion of a tumor
- Marsupialization fails
- It’s a more invasive procedure but definitive.
Procedure Details
- Usually done under local or general anesthesia, depending on the case.
- Performed in a clinic, outpatient surgical center, or hospital.
- Duration: about 30–60 minutes.
Recovery
- Mild discomfort or swelling for a few days
- Most people return to normal activities within a few days to a week
- Abstain from sexual activity and avoid inserting anything vaginally for a few weeks
- Pain relief, antibiotics (if needed), and wound care instructions are provided
Risks and Complications
- Bleeding
- Infection
- Recurrence of the cyst
- Scarring or damage to nearby structures (rare)
Summary
Skene gland cyst surgery is performed to treat cysts near the urethral opening caused by blockage of the Skene (paraurethral) glands. Surgery is recommended when the cyst becomes painful, infected, interferes with urination, or keeps coming back. Common procedures include incision and drainage, marsupialization, or complete excision of the cyst. It is usually a minor, outpatient procedure with a quick recovery and good outcomes.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKİYE



Leave a Reply