Retroperitoneal lymph node dissection (RPLND) is a key surgical procedure used to treat testicular cancer that has spread to the lymph nodes. This surgery invvolves the resection of testicular lymh nodes located in the retroperitoneal area. Here i will try to give general information about RPLND.
What is retroperitoneal lymph node disection?
RPLND is a surgical procedure primarily used in the treatment of testicular cancer. It involves the removal of lymph nodes located in the retroperitoneum, which is the area at the back of the abdominal cavity behind the peritoneum (the lining of the abdominal cavity). These lymph nodes are a common site for the spread (metastasis) of testicular cancer, particularly germ cell tumors.
RPLND can be performed in different contexts:
- Primary RPLND: It aims to remove any remaining cancerous cells and to prevent the spread of the disease.
- Post-chemotherapy RPLND: After a patient undergoes chemotherapy, RPLND may be performed to remove any residual masses in the retroperitoneum. Because chemotherapy may not completely eliminate all cancer cells, and surgery can help ensure that no viable cancer remains.
Indications of RPLND
The primary indications for RPLND include:
- Stage I non-seminomatous germ cell tumors (NSGCT) with High-Risk Features: For patients with clinical stage I NSGCT, RPLND may be indicated if there are high-risk features, such as the presence of lymphovascular invasion, which increase the likelihood of metastasis.
- Stage II NSGCT: Patients with stage II disease have evidence of retroperitoneal lymph node involvement on imaging. RPLND is indicated to remove the affected lymph nodes, particularly if there is a residual mass after chemotherapy, or in cases where chemotherapy is not the initial treatment option.
- Residual mass post-chemotherapy: After chemotherapy, particularly for advanced testicular cancer, residual masses in the retroperitoneum may remain. RPLND is indicated to remove these masses, as they may contain viable cancer cells, teratoma, or necrotic tissue. This is crucial for ensuring a complete response to treatment.
- Persistent or recurrent retroperitoneal mass: If a patient experiences a recurrence of cancer in the retroperitoneal lymph nodes, RPLND may be indicated as part of a salvage treatment strategy.
- Diagnostic uncertainty: In certain cases, RPLND may be indicated when there is diagnostic uncertainty, such as inconclusive imaging or tumor marker levels, to obtain tissue for histopathological examination and confirm the nature of the disease.
- Fertility preservation: In some cases, RPLND may be indicated for fertility preservation. RPLND can be performed in a nerve-sparing manner to reduce the risk of infertility associated with the procedure.
How to do RPLND?
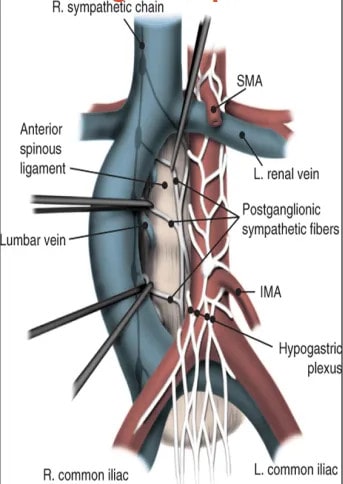
The procedure can be carried out using an open. laparoscopy or robotic surgery. The patient is placed under general anesthesia. The patient is typically positioned supine (lying on the back) with the arms either tucked at the sides or extended outward. A midline abdominal incision is made from just below the sternum (xiphoid process) down to the pubic symphysis to provide access to the retroperitoneal space. The peritoneum is opened, and the intestines are retracted to one side to expose the retroperitoneum. Care is taken to protect surrounding organs and major blood vessels (such as the aorta and inferior vena cava).
Key anatomical structures, including the aorta, inferior vena cava, ureters, and sympathetic nerves, are identified and protected. The dissection is carried out in zones (based on pre-determined templates), which may include the following: On the right side removal of lymph nodes surrounding the inferior vena cava. On the left removal of lymph nodes surrounding the aorta. If needed bialteral removal of lymph nodes on both sides for extensive disease.
What is nerve-sparing RPLD
Nerve-sparing retroperitoneal lymphadenectomy (RPLD) is a surgical procedure used primarily for patients with testicular cancer. It aims to remove retroperitoneal lymph nodes while preserving surrounding nerves, particularly the sympathetic nerves that control ejaculation and sexual function. Whenever possible, the surgeon uses nerve-sparing techniques to preserve the sympathetic nerves that control ejaculation, which is important for fertility preservation.
Complications of RPLND
Here are some of the potential complications associated with RPLND:
- Bleeding
- Injury to surrounding structures:
- Infection
- Lymphocele
- Retrograde ejaculation
- Nerve damage
- Ileus, bowel obstruction
- Deep vein thrombosis (DVT)
- Vascular injury
- Wound complications
- Anesthesia-related complications
- Long-term complications: Infertility and chronic pain:
Post operative follow up after RPLND
Postoperative follow-up after RPLND is critical to monitor the patient’s recovery, assess for complications, and detect any recurrence of cancer.
Immediate postoperative period: Patients usually remain in the hospital for several days following RPLND. Adequate pain control is essential, often involving a combination of medications such as opioids, NSAIDs, and nerve blocks. Early ambulation is encouraged to reduce the risk of DVT and other complications.
Short-term follow-up (first 4-6 weeks): The patient’s incision site should be checked for signs of infection or poor healing. The patient should also be educated on how to care for the wound at home. Patients should be monitored for any symptoms such as fever, significant pain, changes in bowel or urinary function, or signs of lymphocele (e.g., swelling or discomfort in the abdomen). Typically, the first follow-up visit occurs 2-4 weeks after discharge. The surgeon will assess the incision site, review the patient’s recovery, and address any concerns. During this period, the results of the pathological examination of the removed lymph nodes will be reviewed. This information is crucial for determining if further treatment is needed.
Long-term follow-up (6 weeks to 5 years)
- Regular Clinical Visits: Follow-up visits are scheduled every few months for the first two years, then less frequently after that.
- CT Scans: Regular CT scans or MRIs are used to monitor for any recurrence of cancer, typically starting 3-6 months postoperatively and continuing at intervals based on the patient’s risk factors and the findings of previous scans.
- Chest X-Rays: Periodic chest X-rays may be done to check for metastasis to the lungs.
- Tumor Markers (blood tests): Serial measurement of serum tumor markers (e.g., AFP, β-hCG, LDH) is essential to monitor for recurrence or metastasis.
Prognosis after RPLND
The prognosis after RPLND is generally favorable, especially when the procedure is performed as part of a comprehensive treatment plan.
Stage of Cancer: For patients with stage I NSGCT and high-risk features who undergo RPLND, the prognosis is excellent, with cure rates exceeding 95%. Survival rate for Stage II NSGCT patients is typically over 90%, especially if the disease is confined to the lymph nodes and no residual tumor is found after surgery.
Residual Disease After Chemotherapy: For patients who undergo RPLND after chemotherapy, the prognosis depends on the nature of the residual mass. If the mass is composed of teratoma (a benign but potentially aggressive tumor) or necrotic tissue, the prognosis is favorable, with long-term survival rates of around 90%. If viable cancer cells are found in the residual mass, the prognosis is less favorable, but with additional treatments such as salvage chemotherapy or further surgery, many patients still achieve long-term remission.
Histopathological Findings: When RPLND reveals teratoma, the prognosis is generally good, as teratomas are less likely to metastasize but do require removal to prevent future complications. If viable cancer is found during RPLND, additional treatments may be necessary, but the overall survival rate remains high with proper management.
Risk of recurrence: After RPLND, particularly when performed in the absence of residual viable cancer, the recurrence rate is low. The likelihood of recurrence is also influenced by the thoroughness of the lymph node dissection and whether the patient received adjuvant chemotherapy. If recurrence does occur, it is often treatable with additional surgery or chemotherapy.
Long-term survival: In cases of early-stage disease or when RPLND is used as part of multimodal therapy for advanced disease, the cure rate can exceed 90%.
Salvage therapy: Patients who experience a recurrence after RPLND may undergo additional treatments such as salvage chemotherapy or further surgery.
Summary
RPLND is a crucial surgical procedure in the management of testicular cancer, particularly for non-seminomatous germ cell tumors. The procedure is complex, with risks such as retrograde ejaculation and nerve damage, but it offers excellent long-term survival rates, especially when combined with chemotherapy in advanced cases.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply