Vesicovaginal fistula (VVF) is an abnormal connection between the bladder and the vagina, resulting in continuous involuntary leakage of urine into the vaginal vault. This distressing condition primarily affects women’s physical health and quality of life, often carrying significant social and psychological consequences. VVF most commonly arises as a complication of prolonged obstructed labor in low-resource settings, while in more developed regions, it may result from pelvic surgery, radiation therapy, or malignancy. Accurate diagnosis and timely, effective treatment—ranging from conservative management to complex surgical repair—are essential for restoring continence and improving patient outcomes.
What is vesicovaginal fistula?
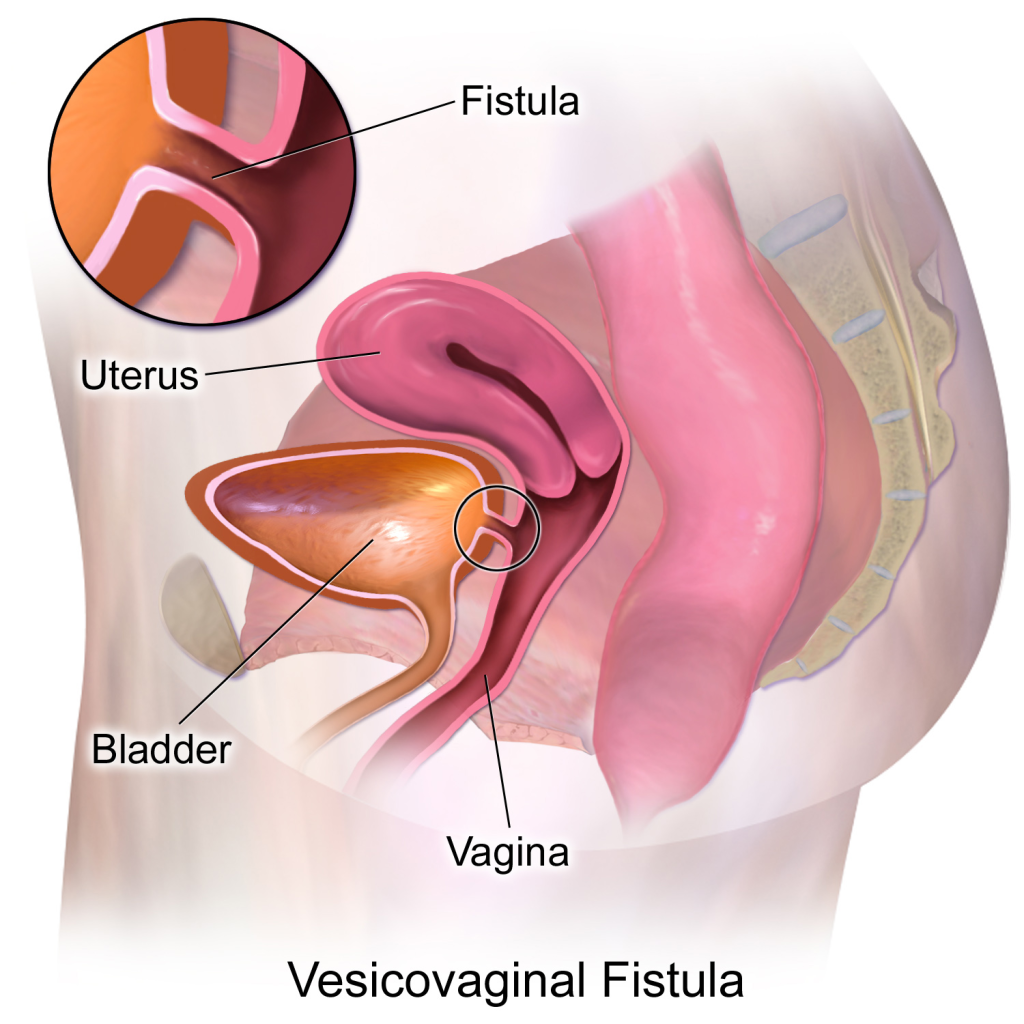
A vesicovaginal fistula is an abnormal opening or tract that forms between the bladder and the vagina, allowing urine to flow continuously and uncontrollably from the bladder into the vaginal canal. This results in persistent urinary leakage, which can be both physically and emotionally distressing for affected individuals.
VVF is a preventable and treatable condition, and with appropriate medical or surgical care, most patients can regain continence and improve their quality of life.
Causes of vesicovaginal fistula
The causes of VVF can vary depending on geographical, healthcare, and social contexts. They are generally classified as obstetric, surgical, radiation-related, malignant, or traumatic. Here’s an overview of the most common causes:
Obstetric Causes
- Prolonged obstructed labor: This is the leading cause in low-resource settings. Prolonged pressure of the fetal head against the pelvic organs leads to tissue necrosis (death), resulting in fistula formation.
- Inadequate obstetric care: Lack of timely cesarean delivery or skilled birth attendance increases the risk.
Surgical Causes
- Hysterectomy (removal of the uterus): The most common surgical cause in developed countries. Inadvertent injury to the bladder during surgery can lead to VVF.
- Pelvic surgeries: Operations involving the bladder, vagina, or reproductive organs may result in accidental damage and fistula formation.
Radiation Therapy
- Used to treat pelvic cancers (e.g., cervical, bladder, or rectal cancer), radiation can cause tissue damage and necrosis, leading to fistula development months or years later.
Malignancy
- Advanced cervical, bladder, or vaginal cancer can directly erode into the bladder and vagina, forming a fistula.
Trauma
- Pelvic fractures or penetrating injuries (e.g., from accidents or sexual violence) can result in VVF.
- Foreign bodies inserted into the vagina may also lead to tissue breakdown and fistula formation.
Infection and Inflammatory Diseases
- Though rare, severe infections or chronic inflammatory conditions such as tuberculosis or Crohn’s disease can contribute to fistula formation.
Symptoms
The primary symptom of a VVF is continuous, involuntary leakage of urine from the vagina, but several other symptoms may also occur depending on the size and location of the fistula, as well as any associated infections or complications.
Common Symptoms:
Continuous urinary leakage through the vagina: This is the hallmark symptom, often occurring without any warning or control.
Wetness and irritation in the vaginal and perineal area: Constant moisture can cause skin breakdown, rashes, and discomfort.
Foul-smelling vaginal discharge: May be due to infection or persistent urine contact.
Recurrent urinary tract infections (UTIs): Due to the abnormal flow of urine and possible bacterial contamination.
Pain or discomfort: Some women may experience pelvic or vaginal pain, particularly if infection or inflammation is present.
Vaginal inflammation or burning sensation: Caused by urine irritating the vaginal mucosa.
Social and emotional distress: The condition often leads to embarrassment, social isolation, depression, and anxiety.
Amenorrhea or infertility (in cases related to childbirth injury): Especially if associated injuries to reproductive organs are present.
These symptoms usually appear within days to weeks after the underlying cause (e.g., childbirth, surgery, radiation) and require prompt medical evaluation for diagnosis and treatment.
Diagnosis
Diagnosis of VVF involves a combination of clinical evaluation, imaging, and sometimes endoscopic procedures to confirm the presence, size, and location of the fistula. Accurate diagnosis is crucial for effective treatment planning.
Medical History and Physical Examination: History: Continuous urine leakage, especially after childbirth, pelvic surgery, or radiation.
Pelvic examination: A speculum exam may reveal visible leakage of urine from the vaginal wall or the fistula opening.
Dye Tests: These are simple and effective bedside tests:
- Methylene blue test (three-swab test):
- Methylene blue is instilled into the bladder via a catheter.
- Swabs placed in the vagina are checked for blue staining.
- If blue dye appears on the swabs, a vesicovaginal fistula is likely.
- Double dye test:
- Involves oral phenazopyridine (colors urine orange) and methylene blue in the bladder.
- Helps differentiate between vesicovaginal and ureterovaginal fistulas.
Cystoscopy: A thin, lighted scope (cystoscope) is inserted through the urethra into the bladder. Allows direct visualization of the bladder interior and fistula opening.
Imaging Studies: Voiding cystourethrogram (VCUG), CT or MRI urography, Ultrasound.
Intravenous Urography (IVU): Helps assess the upper urinary tract and rule out ureteral involvement.
Vaginoscopy: Similar to cystoscopy, but focused on examining the vaginal side of the fistula.
Surgery of vesicovaginal fistula/treatment
Surgical repair is the mainstay treatment for most vesicovaginal fistulas, especially when the fistula does not close with conservative measures. The goal of surgery is to close the fistulous tract, restore normal urinary function, and prevent recurrence.
Timing of Surgery
- Early repair: May be attempted in select cases, especially small fistulas detected early after injury.
- Delayed repair: Preferred in most cases—after 3–6 months—to allow inflammation and infection to subside and tissues to become healthier.
Surgical Approaches
Transvaginal Approach
- Most commonly used for low-lying fistulas.
- Advantages: Less invasive, faster recovery, less blood loss.
- Procedure:
- The fistula is accessed through the vagina.
- The tract is excised or de-epithelialized.
- The bladder and vaginal walls are closed in multiple layers, often with interposition of healthy tissue (e.g., Martius flap—a fatty tissue flap from the labia).
Transabdominal Approach
- Used for high, complex, or recurrent fistulas, or when vaginal access is limited.
Can be performed as: Open surgery, laparoscopic, robotic-assisted
- Procedure:
- Bladder is opened from above, fistula is excised, and repair is done in layers.
- A tissue interposition flap (e.g., omentum, peritoneum) may be used to strengthen the repair.
Laparoscopic/Robotic Surgery
- Minimally invasive options that offer:
- Better visualization
- Shorter hospital stays
- Faster recovery
- Require specialized training and equipment.
Postoperative Care
- Bladder drainage via Foley catheter for 10–14 days to allow healing.
- Antibiotics to prevent infection.
- Avoidance of vaginal intercourse or strenuous activity for 6–8 weeks.
When Surgery May Not Be Feasible
- Patients who are not fit for surgery
- Extensive cancer or radiation damage
- In such cases, urinary diversion (e.g., ileal conduit) may be considered as a last resort.
Follow-up after surgery
Postoperative follow-up is essential to ensure successful healing, monitor for complications, and support the patient’s physical and emotional recovery. A structured follow-up plan increases the likelihood of a good outcome and minimizes the risk of recurrence.
1. Immediate Postoperative Period
- Bladder drainage: A Foley catheter is typically left in place for 10 to 14 days (or longer if needed) to keep the bladder decompressed and allow the repair site to heal without tension.
- Antibiotics and pain management: To prevent infection and relieve discomfort.
- Monitoring for signs of complications, such as:
- Persistent urinary leakage
- Fever or infection
- Pain or hematuria (blood in urine)
2. Catheter Removal and Assessment
- Catheter trial removal: Usually after 2 weeks.
- Voiding trial: To assess bladder capacity and continence.
- Dye test (e.g., methylene blue test) may be repeated to ensure no leakage from the repair site.
3. Follow-Up Visits
Scheduled follow-up visits typically occur at:
- 2 weeks (after catheter removal)
- 6 weeks
- 3 months
- 6 months
- Annually, if needed
During follow-up visits, the physician may:
- Perform a pelvic exam to assess healing.
- Check for recurrent fistula, infection, or scar tissue.
- Evaluate for bladder dysfunction, such as urgency or incontinence.
4. Imaging and Cystoscopy
- If symptoms persist or recur, cystoscopy or imaging studies (e.g., cystogram, MRI) may be needed to rule out recurrence or new fistulas.
5. Patient Education and Counseling
- Advice on fluid intake, perineal hygiene, and sexual activity (usually delayed for 6–8 weeks).
- Psychological support if needed, especially in women who experienced social stigma or trauma related to VVF.
- Family planning counseling if applicable.
6. Pelvic Floor Rehabilitation
- Pelvic floor exercises may help regain continence and strengthen the pelvic muscles.
- Referral to a urogynecologist or pelvic floor therapist may be beneficial in complex cases.
7. Long-Term Monitoring
Some patients may require:
- Continued urological care, especially after radiation or cancer-related fistulas.
Success rate of surgery
The success rate of surgical repair for VVF is generally high but varies depending on several factors such as the size and location of the fistula, the cause, the timing of repair, the surgical technique used, and the surgeon’s experience.
General Success Rates:
- Primary repair success:
Most studies report a success rate between 85% and 95% for first-time (primary) surgical repairs. - Repeat or complex repairs:
Success rates tend to be lower, around 70% to 85%, especially for large, recurrent, or radiation-related fistulas. - Timing impact:
Delayed repairs (after inflammation has settled) usually have better outcomes compared to immediate repairs.
Factors Influencing Success:
- Fistula size: Smaller fistulas have higher success rates.
- Fistula location: Low vaginal fistulas are generally easier to repair than high or complex fistulas.
- Tissue quality: Healthy, well-vascularized tissue improves healing.
- Cause: Obstetric fistulas tend to have better outcomes than those caused by radiation or malignancy.
- Surgical approach: Skilled surgeons and specialized centers tend to report better results.
- Postoperative care: Proper bladder drainage and infection control contribute to success.
Summary:
| Condition | Success Rate (%) |
| Primary VVF repair | 85 – 95 |
| Complex or recurrent fistula repair | 70 – 85 |
| Radiation-related fistulas | Lower, variable |
Summary
VVF is an abnormal connection between the bladder and vagina causing continuous urinary leakage, often resulting from prolonged obstructed labor, pelvic surgery, or radiation. Diagnosis involves clinical evaluation, dye tests, cystoscopy, and imaging to confirm the fistula’s presence and location. Treatment primarily consists of surgical repair, either through vaginal or abdominal approaches, with high success rates especially when performed by experienced surgeons. Timely diagnosis and appropriate management are crucial to restore continence, improve quality of life, and reduce physical and social complications associated with VVF.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply