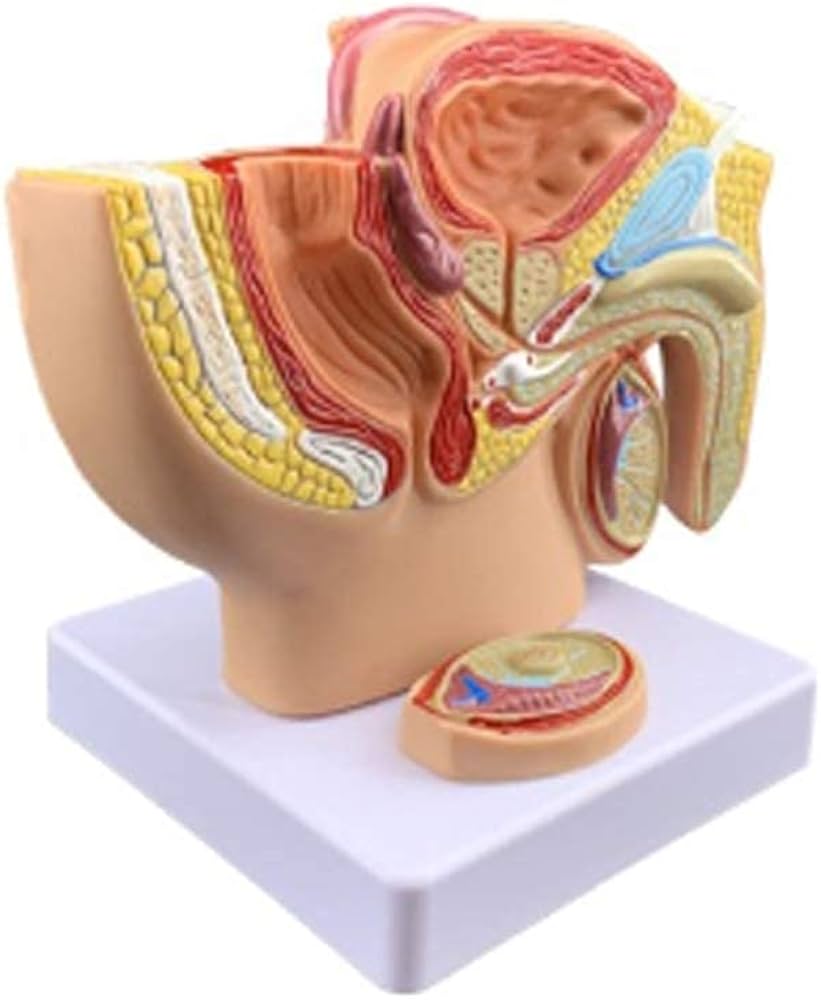
Andrology is a specialized branch of medicine focused on the male reproductive system and its associated disorders. It involves the study, diagnosis, and treatment of conditions related to male fertility, sexual health, and hormonal imbalances. Andrologic diseases include a range of conditions such as erectile dysfunction, male infertility, testosterone deficiency, and prostate disorders. Andrologic procedures are medical or surgical interventions aimed at treating these conditions, improving male reproductive health, and enhancing quality of life for affected individuals.
What is andrology?
Andrology is a branch of medicine that focuses on the male reproductive system, its health, and related disorders. It deals with issues such as male infertility, erectile dysfunction, testosterone imbalances, and other conditions that affect the male reproductive organs, including the prostate and testes. Andrologists specialize in diagnosing and treating these conditions, aiming to improve men’s sexual and reproductive health. This field is similar to gynecology, which focuses on the female reproductive system, but with a focus on male physiology and conditions.
What are the andrological diseases?
Here are some common andrological diseases:
- Erectile Dysfunction
- Male Infertility
- Low Testosterone (Hypogonadism)
- Prostate Disorders (e.g., Benign Prostatic Hyperplasia, Prostatitis)
- Peyronie’s Disease
- Varicocele
- Hyperspermia
- Azoospermia
- Orchitis
- Epididymitis
- Testicular Cancer
- Klinefelter Syndrome
- Male Hypogonadism
- Sexual Dysfunction (e.g., Premature Ejaculation, Delayed Ejaculation)
- Priapism
What are the andrological diagnostic methods?
Here are common andrological diagnostic methods used to evaluate male reproductive and sexual health:
- Physical Examination
- Semen Analysis
- Hormonal Blood Tests (e.g., testosterone, LH, FSH, prolactin)
- Scrotal Ultrasound
- Penile Doppler Ultrasound
- Testicular Biopsy
- Genetic Testing (e.g., karyotyping, Y chromosome microdeletion)
- Urinalysis and Urine Culture
- Nocturnal Penile Tumescence (NPT) Test
- Prostate-Specific Antigen (PSA) Test
- Transrectal Ultrasound (TRUS)
- MRI or CT Scan (in specific cases)
- Sperm DNA Fragmentation Test
- Post-ejaculation Urinalysis
- Psychological Evaluation (for psychogenic erectile or sexual dysfunction)
These tests help identify the underlying causes of andrological diseases and guide appropriate treatment.
Classical and new treatment methods in andrology
Classical Treatment Methods:
- Pharmacological Therapies:
- Phosphodiesterase Inhibitors (e.g., Sildenafil, Tadalafil) – for erectile dysfunction
- Hormone Replacement Therapy (e.g., Testosterone) – for hypogonadism
- Antibiotics – for infections like prostatitis or epididymitis
- Anti-inflammatory Medications – for chronic pelvic pain syndrome
- Surgical Treatments:
- Varicocelectomy (microscopic varicocelectomy, microsurgery) – for varicocele-related infertility
- Vasectomy/Vasovasostomy – for sterilization or reversal
- Testicular Sperm Extraction (TESE) – for azoospermia
- Penile Prosthesis Implantation – for severe erectile dysfunction
- Circumcision – for phimosis or recurrent infections
- Assisted Reproductive Techniques (ART):
- Intrauterine Insemination (IUI)
- In Vitro Fertilization (IVF)
- Intracytoplasmic Sperm Injection (ICSI)
- Lifestyle Modifications:
- Smoking cessation, weight loss, exercise, stress reduction, and diet changes
New and Emerging Treatment Methods:
- Regenerative Medicine:
- Platelet-Rich Plasma (PRP) Therapy – for erectile dysfunction
- Stem Cell Therapy – experimental use in erectile dysfunction and infertility
- Shockwave Therapy (Li-ESWT) – low-intensity extracorporeal shockwave therapy for erectile dysfunction
- Gene Therapy:
- Investigational treatments targeting genetic causes of infertility or hypogonadism
- Advanced Hormonal Modulation:
- Selective Estrogen Receptor Modulators (SERMs)
- Aromatase Inhibitors – used in male infertility related to hormonal imbalance
- Robotic and Minimally Invasive Surgeries:
- Robotic-assisted varicocelectomy or prostate surgery
- New Drug Formulations:
- Long-acting testosterone therapies
- Topical testosterone gels and nasal testosterone delivery
- Digital and Wearable Technologies:
- Tools for monitoring erectile function, hormone levels, or semen parameters at home (emerging field)
These classical and cutting-edge methods are often combined and tailored based on individual patient needs to optimize outcomes in andrological care.
Molecular treatment methods in andrology
Molecular treatments in andrology focus on targeting the underlying cellular and genetic mechanisms involved in male reproductive and sexual health disorders. These approaches are still emerging but show great promise in advancing personalized and effective treatments.
1. Gene Therapy
- Purpose: Correct genetic defects responsible for male infertility or hormonal dysfunction.
- Applications:
- Treating Y chromosome microdeletions
- Addressing mutations in genes related to spermatogenesis
- Potential future use in correcting androgen receptor defects in androgen insensitivity syndromes
2. Stem Cell Therapy
- Purpose: Regenerate damaged tissues, particularly in testicular or erectile tissues.
- Types Used:
- Mesenchymal stem cells (MSCs)
- Adipose-derived stem cells
- Applications:
- Erectile dysfunction (ED)
- Testicular failure
- Restoration of spermatogenesis in non-obstructive azoospermia
3. Platelet-Rich Plasma (PRP) Therapy
- Molecular Basis: PRP is rich in growth factors (e.g., VEGF, PDGF, TGF-β) that stimulate tissue repair and angiogenesis.
- Application: Used in erectile dysfunction to improve penile vascularization and nerve regeneration.
4. RNA-based Therapies
- Purpose: Regulate gene expression or silence disease-related genes.
- Types:
- siRNA (small interfering RNA)
- miRNA (microRNA) modulation
- Applications: Under research for controlling testicular inflammation, apoptosis in testicular tissue, and hormone signaling pathways.
5. Hormonal Receptor Modulators
- Target: Androgen receptors and related signaling pathways.
- Examples:
- Selective Androgen Receptor Modulators (SARMs)
- Androgen receptor gene editing (experimental)
6. Antioxidant and Enzyme Modulation at the Molecular Level
- Purpose: Reduce oxidative stress in sperm and reproductive tissues.
- Agents:
- Coenzyme Q10
- Glutathione
- Enzyme modulators like catalase, superoxide dismutase (SOD) mimetics
7. Epigenetic Therapies (Emerging Area)
- Focus: Modify DNA methylation, histone acetylation to improve sperm quality and restore fertility.
- Potential Uses:
- Environmental or idiopathic infertility
- Aging-related sperm DNA damage
These molecular therapies represent a promising future in andrology, especially for conditions like idiopathic infertility, erectile dysfunction unresponsive to standard treatments, and genetic disorders. Most are still in the research or clinical trial phase but hold the potential for highly personalized and effective treatments.
Future of andrology: Key trends and emerging directions
The future of andrology is shaped by rapid advances in molecular biology, regenerative medicine, biotechnology, and digital health. These developments promise more personalized, effective, and less invasive treatments for male reproductive and sexual health issues.
1. Personalized and Precision Medicine
- Genomic Profiling: Identifying genetic causes of infertility and sexual dysfunction for tailored treatments.
- Pharmacogenomics: Using a patient’s genetic makeup to predict response to andrological drugs (e.g., testosterone therapy).
- Biomarker Development: Discovery of molecular markers for early detection of testicular dysfunction, prostate disease, and sperm quality.
2. Regenerative and Molecular Therapies
- Stem Cell Therapy: Clinical applications for restoring spermatogenesis and treating erectile dysfunction.
- Gene Editing (e.g., CRISPR-Cas9): Potential to correct genetic mutations responsible for male infertility and hormonal disorders.
- RNA Therapies: Use of siRNA/miRNA to regulate hormone levels, spermatogenesis, and tissue repair.
- Epigenetic Interventions: Addressing sperm DNA methylation and histone modification for fertility restoration.
3. Technological Integration
- Robotic and Minimally Invasive Surgery: Precision surgeries for varicocele, prostate, or penile implants.
- AI and Machine Learning: For analyzing semen parameters, predicting fertility outcomes, and optimizing treatment decisions.
- 3D Bioprinting: Future use in tissue engineering, including artificial testicular or penile tissues.
4. Digital Health and Telemedicine
- Remote Monitoring: Wearable tech for tracking erectile function or hormone levels.
- Mobile Apps: For managing medications, sexual health assessments, and fertility tracking.
- Teleandrology: Expanding access to care through virtual consultations and at-home diagnostic kits.
5. Holistic and Preventive Approaches
- Male Fertility Preservation: Increased focus on sperm banking and fertility care for cancer survivors.
- Lifestyle and Environmental Factors: Research into how diet, toxins, and stress affect male fertility and sexual function.
- Integrative Therapies: Combining traditional and modern approaches for chronic pelvic pain or psychosomatic sexual disorders.
Conclusion
The future of andrology is moving toward highly personalized, minimally invasive, and technologically advanced care. As understanding of the molecular basis of male reproductive health deepens, andrology will play a key role in addressing not just fertility and sexual function, but overall male wellness and longevity.
Summary
Andrology is the medical specialty focused on male reproductive and sexual health. It deals with diagnosing and treating andrologic diseases such as erectile dysfunction, male infertility, low testosterone, and prostate disorders. Andrologic procedures include both diagnostic and therapeutic interventions like semen analysis, hormone testing, varicocelectomy, penile implants, and assisted reproductive techniques, all aimed at improving male reproductive function and quality of life.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply