“Inguinal lymphadenitis, also known as inguinal lymphadenopathy, refers to the swelling and inflammation of lymph nodes located in the groin area, known as inguinal nodes. This condition typically occurs as a response to an infection or inflammation in the lower extremities, genitalia, or pelvic region. Common causes include sexually transmitted infections (STIs) such as gonorrhea or chlamydia, skin infections, or even systemic infections originating elsewhere in the body. Symptoms may include pain, tenderness, warmth, and swelling in the groin area. Treatment focuses on addressing the underlying cause with antibiotics or other appropriate therapies, alongside symptomatic relief measures such as rest and pain management.”
What is “inguinal lympadenitis/lymphadenopathy”
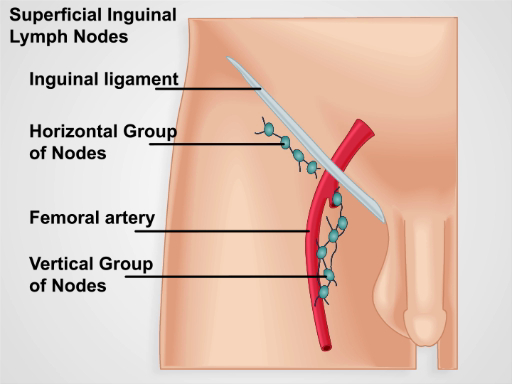
“Inguinal lymphadenitis or lymphadenopathy refers to the enlargement or inflammation of lymph nodes located in the inguinal region, which is the area where the upper thigh meets the lower abdomen, commonly known as the groin. Lymphadenitis specifically denotes inflammation of the lymph nodes, while lymphadenopathy refers to their abnormal enlargement.
Causes
Inguinal lymphadenitis or lymphadenopathy can have various causes, including:
Infections:
- Bacterial Infections: Common bacterial causes include infections from skin wounds, cellulitis (skin infection), or infections spread through the lymphatic system from lower extremities or genitalia.
- Sexually Transmitted Infections (STIs): Gonorrhea and chlamydia are notable STIs that can cause inguinal lymphadenitis due to their involvement with the genital and pelvic regions.
- Tuberculosis: In some cases, tuberculosis (TB) can lead to the enlargement of inguinal lymph nodes.
- Fungal Infections: Fungal infections such as candidiasis or tinea cruris (jock itch) can also cause lymphadenitis in the groin area.
Non-infectious Inflammatory Conditions:
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease or ulcerative colitis can lead to lymphadenopathy as part of the inflammatory process.
- Rheumatoid Arthritis: Inflammatory arthritis can sometimes cause generalized lymphadenopathy, including inguinal involvement.
- Sarcoidosis: This systemic inflammatory disease can affect multiple organs, including causing lymph node enlargement.
Malignancies:
- Lymphoma: Both Hodgkin’s lymphoma and non-Hodgkin’s lymphoma can cause lymphadenopathy, including in the inguinal region.
- Metastatic Cancer: Cancer from other parts of the body (such as melanoma, prostate, or gynecological cancers) can spread to the inguinal lymph nodes.
Autoimmune Disorders:
- Some autoimmune conditions like systemic lupus erythematosus (SLE) or Sjögren’s syndrome can lead to generalized lymphadenopathy.
Other Causes:
- Medications: Certain medications can occasionally cause lymphadenopathy as a side effect.
- Insect Bites: Occasionally, insect bites or other forms of localized irritation can lead to inguinal lymph node enlargement.
Symptoms
Inguinal lymphadenopathy refers to the abnormal enlargement of lymph nodes located in the groin area, known as inguinal nodes. The symptoms can vary depending on the underlying cause but commonly include:
- Swelling: The affected lymph nodes in the groin area may become noticeably enlarged. This swelling can range from mild to pronounced.
- Tenderness or Pain: The enlarged lymph nodes may be tender to the touch or painful, especially when pressure is applied.
- Warmth and Redness: The skin overlying the swollen lymph nodes may appear red and feel warm to the touch. This is often indicative of inflammation in the area.
- Discomfort or Sensation of Fullness: Some individuals may experience a feeling of heaviness, fullness, or discomfort in the groin area due to the enlarged lymph nodes.
- Difficulty Moving or Flexing: In severe cases of inguinal lymphadenopathy, the swelling and inflammation can limit movement or flexibility in the groin and thigh region.
- Fever: Depending on the cause of the lymphadenopathy, fever may accompany the swelling and indicate an underlying infection.
- Other Systemic Symptoms: If the lymphadenopathy is due to a systemic infection or disease, additional symptoms such as fatigue, weight loss, night sweats, or generalized malaise may be present.
Diagnosis
Diagnosing inguinal lymphadenopathy involves a systematic approach that includes several steps:
Medical History and Physical Examination:
- A detailed history helps identify symptoms such as swelling, pain, tenderness, and any associated systemic symptoms like fever or weight loss.
- The physical examination focuses on assessing the size, location, consistency (soft or hard), tenderness, and mobility of the enlarged lymph nodes in the groin area.
Laboratory Tests:
- Complete Blood Count (CBC): Helps assess for signs of infection or inflammation, such as elevated white blood cell count (leukocytosis) or changes in differential counts.
- Inflammatory Markers: Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be elevated in cases of inflammatory causes.
- Serological Tests: Depending on the suspected cause, tests for specific infections such as HIV, syphilis, Epstein-Barr virus, or other pathogens may be performed.
Imaging Studies:
- Ultrasound: Often the initial imaging modality of choice to evaluate the size, number, and characteristics of the enlarged lymph nodes in the inguinal region. Ultrasound helps differentiate between benign and malignant causes and can guide further evaluation.
- CT Scan or MRI: These imaging techniques provide more detailed information about the lymph nodes and surrounding structures, particularly useful when assessing for spread of infection or signs of malignancy.
Biopsy and Histopathological Examination:
- Fine-Needle Aspiration (FNA) Biopsy: A thin needle is used to obtain a sample of cells from the enlarged lymph node for microscopic examination. FNA biopsy is less invasive and can provide valuable diagnostic information, such as determining if the cause is infectious, inflammatory, or malignant.
- Excisional Biopsy: In cases where FNA biopsy is inconclusive or malignancy is suspected, a surgical excisional biopsy may be necessary to remove the entire lymph node or a portion of it for thorough examination by a pathologist.
Microbiological Cultures and Tests:
- Cultures of aspirated fluid or tissue may be performed to identify specific pathogens, especially in cases of suspected bacterial or fungal infections.
Specialized Evaluations:
- Depending on the initial findings and suspected cause, referral to specialists such as infectious disease specialists, hematologists (blood disorder specialists), or oncologists (cancer specialists) may be warranted for further evaluation and management.
Treatment
The treatment of inguinal lymphadenopathy depends on the underlying cause identified through diagnostic evaluation. Here are some general approaches based on common causes:
Infections:
- Bacterial Infections: Treatment typically involves antibiotics targeted against the specific bacteria causing the infection. Common antibiotics may include penicillin derivatives, cephalosporins, or macrolides. The choice of antibiotic depends on the suspected or identified pathogen and its sensitivity profile.
- Viral Infections: Treatment is often supportive, focusing on rest, hydration, and symptom management. Antiviral medications may be used in specific viral infections such as herpes simplex virus (HSV), cytomegalovirus (CMV), or HIV.
- Fungal Infections: Antifungal medications such as fluconazole or itraconazole may be prescribed depending on the type of fungal infection identified.
- Inflammatory Conditions:
- Treatment depends on the underlying inflammatory disorder. For autoimmune diseases like rheumatoid arthritis or systemic lupus erythematosus (SLE), treatment may involve corticosteroids, immunosuppressive medications (e.g., methotrexate), or biologic therapies to reduce inflammation and manage symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may also be used to alleviate pain and inflammation associated with inflammatory causes of lymphadenopathy.
Malignancies:
- Treatment is guided by the type and stage of cancer. It may include chemotherapy, radiation therapy, surgery (e.g., lymph node dissection), targeted therapies, or a combination of these modalities. Referral to an oncologist is crucial for specialized management and treatment planning.
Supportive Care:
- Regardless of the cause, supportive care measures such as rest, adequate hydration, and pain management (e.g., acetaminophen or NSAIDs) may help alleviate symptoms associated with inguinal lymphadenopathy.
- Warm compresses or local measures may be used to relieve discomfort and promote healing, especially in cases of mild lymphadenopathy.
Monitoring and Follow-Up:
- Regular follow-up visits with a healthcare provider are important to monitor the response to treatment, assess for complications, and adjust the treatment plan as needed based on clinical progress and follow-up imaging or laboratory tests.
Surgical Intervention:
- In some cases, surgical intervention may be necessary for diagnostic purposes (biopsy) or therapeutic purposes (e.g., excision of persistent or suspicious lymph nodes).
Education and Prevention:
- Educating patients about the importance of completing prescribed courses of antibiotics or medications, maintaining good hygiene practices, and avoiding exposure to known risk factors (e.g., unprotected sexual contact) can help prevent recurrence or spread of infectious causes of lymphadenopathy.
Summary
Inguinal lymphadenitis or lymphadenopathy refers to the swelling and inflammation of lymph nodes located in the groin area. It typically occurs in response to infections, such as sexually transmitted infections (STIs) like gonorrhea or chlamydia, skin infections, or systemic illnesses. Symptoms include swelling, tenderness, warmth, and sometimes fever. Diagnosis involves medical history, physical examination, imaging (like ultrasound), and possibly biopsy. Treatment depends on the underlying cause and may include antibiotics for infections, anti-inflammatory medications for autoimmune conditions, or specific therapies for malignancies.
Prof. Dr. Emin ÖZBEK
Urologist
Istanbul- TURKIYE


Leave a Reply